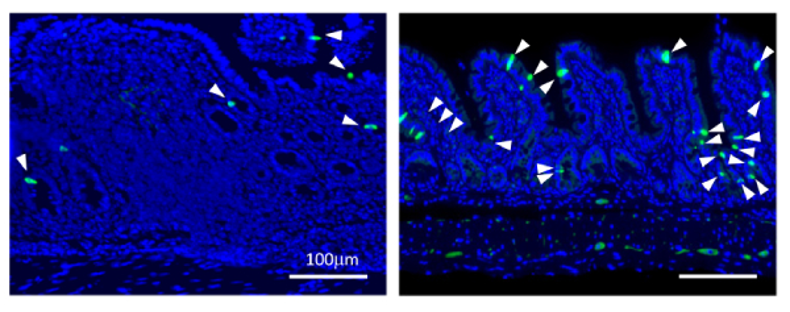
Researchers at Vanderbilt University have, for the first time, been able to trigger the specific immune system response required to reverse the course of small intestinal inflammation by inducing production of tuft cells, very rare epithelial cells that sense and respond to parasites. The breakthrough has the potential to provide Crohn’s disease and inflammatory bowel disease patients a safe alternative to what’s known as helminthic therapy, wherein parasitic organisms are introduced to the body to stimulate an immune response and calm inflammation.
The article “Succinate Produced by Intestinal Microbes Promotes Specification of Tuft Cells to Suppress Ileal Inflammation” was published online in the journal Gastroenterology on Aug. 24.
During the past five years, there has been a flurry of scientific research around tuft cells—a cell type comprising less than 1 percent of all the cells forming the outer lining of the intestinal tract—adding to widespread scientific knowledge of the cell’s phenotype over the past half century. Despite five decades of study, this research, conducted by Ken Lau, associate professor of cell and developmental biology, and former graduate student Amrita Banerjee, is the first that looks into how tuft cells can specifically address symptoms of CD and IBD.

To determine the number of tuft cells needed to trigger an immune response to inflammation, the researchers first sought to understand the process that stimulates tuft cell generation. By deploying single-cell RNA sequencing and microbiome analysis, they determined that the microbiome can stimulate tuft cell generation in a positive feedback loop through specific molecules. When this strategy was applied to CD, increasing tuft cell numbers ultimately reversed the course of intestinal inflammation.
“We are in the era of single-cell biology, a time when we are able to more fully comprehend the importance of rare cell populations with respect to the body’s overall health and have the tools to study them,” Lau said. “We have seen evidence that administering this technique as a therapeutic strategy reverses the course of intestinal inflammation. Next we will be looking closely at the mechanisms that enable tuft cells’ functionality and how it can be clinically applied.”
Added Banerjee, “Without much known about this rare type of cell, we have been able to answer fundamental questions about how they are produced. Using this research to address human disease was a goal of mine as a student, and to realize it has been a highly rewarding experience. We have been able to apply a gamut of techniques to our research and then walk from the lab to the clinic to evaluate the human impact of our work. The Vanderbilt community has provided so many intentional and serendipitous contributions to this research.”
The synergy between the collaborators has resulted in a provisional patent application that Lau worked on with the Center for Technology Transfer and Commercialization.
During her time working in Lau’s lab, Banerjee was a science policy and programming intern at Life Science Tennessee, a nonprofit dedicated to advancing the life science industry through advocacy and partnerships. Currently, she is serving as an American Association for the Advancement of Science Science and Technology Policy Fellow. Over the course of this fellowship for outstanding scientists, Banerjee will work with a member of Congress to develop firsthand knowledge of policy making and advocacy for science funding at the federal level.
“Working within the complexity of how a single cell functions within a system has always been exciting for me,” said Banerjee. “To apply the same kind of thinking, how individuals can make broad policy impacts and improve human health, is an experience I am very much looking forward to.”
The research was funded in part by the National Institute of Diabetes and Digestive and Kidney Diseases (grants R01DK103831 and P30DK058404), the National Institute of Allergy and Infectious Diseases (grant T32Al138932), the National Cancer Institute (grant P50CA236733), the Vanderbilt Microbiome Initiative and Cure for IBD.