Researchers at Vanderbilt University Medical Center, in collaboration with Seaside Therapeutics in Cambridge, Mass., have achieved a milestone in the development of a potential new treatment for fragile X syndrome, the most common genetic cause of autism.
Drug-like molecules developed at Vanderbilt are undergoing the final pre-clinical studies required by the FDA before entering clinical testing at Seaside Therapeutics and could be ready for human testing in early 2012, said Jeffrey Conn, co-director of the Vanderbilt Center for Neuroscience Drug Discovery and a member of Seaside Therapeutics’ advisory board.
Vanderbilt also is participating in clinical trials of another drug candidate developed by Seaside Therapeutics called STX209 (arbaclofen), which may decrease social withdrawal, a core symptom found in people with fragile X syndrome and autism spectrum disorders (ASD).
“Seaside Therapeutics has partnered with Vanderbilt and other leading academic institutions to translate breakthrough discoveries in neurobiology into therapeutics that we believe will address the underlying causes of these disorders and, in turn, offer the greatest potential to improve the lives of patients and their families,” said Randall Carpenter, president and chief executive officer of Seaside Therapeutics.
Fragile X most common genetic cause of autism
Fragile X syndrome, also the most common inherited form of intellectual and developmental disabilities, is relatively rare, affecting approximately 90,000 people in the United States. Major symptoms include impaired cognitive function, developmental delay, attention deficit and hyperactivity, anxiety, obsessive-compulsive and autistic behaviors.

Research conducted by the founders of Seaside Therapeutics and others suggest that excessive signaling through a receptor called mGluR5, which binds the neurotransmitter glutamate, may contribute to manifestations of fragile X syndrome.
In 2008, Seaside Therapeutics awarded Vanderbilt a $4.5 million grant to develop drug-like compounds that can improve fragile X symptoms by “tuning down” receptor activity. Last year, they began a second collaboration to discover and develop other classes of compounds that may be effective in treating the disorder. The National Institutes of Health also supported many of the studies that provided the groundwork for the Seaside-Vanderbilt collaboration.
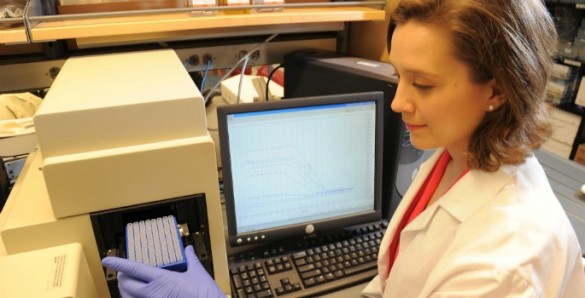
Conn’s colleagues in this effort included Craig Lindsley, co-director in the Center for Neuroscience Drug Discovery and director of medicinal chemistry; Carrie Jones, the center’s director of in vivo pharmacology; Colleen Niswender, director of molecular pharmacology, J. Scott Daniels, director of drug metabolism and pharmacokinetics, Kyle Emmitte, research assistant professor of pharmacology and medicinal chemistry lead, and Alice Rodriguez, instructor in pharmacology.
Researchers fill vital drug pipeline
It can cost over a billion dollars to bring a drug to market. Cuts in health care reimbursement for medications could make it even more difficult for pharmaceutical companies to recoup that investment. Some firms already are downsizing their research operations as patent protection ends for some of their best-selling brand name products.
The rapid progress made by the Seaside Therapeutics-Vanderbilt partnership exemplifies how academic medical centers can help to fill the “drug pipeline” with new agents that potentially may improve the health of millions of patients worldwide.