Audrey Bowden, Dorothy J. Wingfield Phillips Chancellor’s Faculty Fellow and associate professor of biomedical and electrical engineering, has won a grant from the National Institute of Biomedical Imaging and Bioengineering to develop a novel noninvasive smartphone-integrated device to provide accurate, point-of-care detection of jaundice in newborns of all skin tones.

Newborns have immature liver function that is inefficient at metabolizing bilirubin, a yellowish pigment that is made during the normal breakdown of red blood cells. Consequently, nearly 80 percent of preterm and 60 percent of term babies develop hyperbilirubinemia, a potentially fatal form of neonatal jaundice, within a week of their birth. The gold standard for detecting hyperbilirubinemia is the use of frequent blood tests to measure bilirubin levels, but this approach is expensive and painful and increases likelihood of infection.
Existing noninvasive methods to monitor hyperbilirubinemia are not yet fully able to replace blood tests, though some are clinically accepted for jaundice screening. These tests yield acceptable results in light-skinned newborns but have low correlation for clinical decision-making in dark-skinned newborns and low availability in low- and middle-income countries.
“Noninvasive jaundice testing technologies are not able to detect jaundice well in dark-skinned newborns because when light enters the body, it has to go through the skin to reach what the light is testing: all the molecules and blood within the body. For dark-skinned individuals, this can include substantial contributions from melanin, which are not accounted for in the design of existing technologies for noninvasive jaundice testing,” Bowden said.
“In the case of a jaundiced newborn, we need tests that can discriminate between light that has been affected by skin tone and light that came directly from the blood. If tests have spectral cross-talk, or mixed signals that have not accounted for skin tone effects, skin tone can give clinicians false results.”
Bowden and her team are developing a technology that uses light in a way that can penetrate through the skin. With her expertise in light-based technologies, Bowden will use optical coherence tomography, a technique with the ability to segment out light that comes back from the skin from light that comes back from the blood. “Our expectation is that if we’re able to isolate light information from the blood, it will be similarly effective to conducting a blood test,” Bowden said.
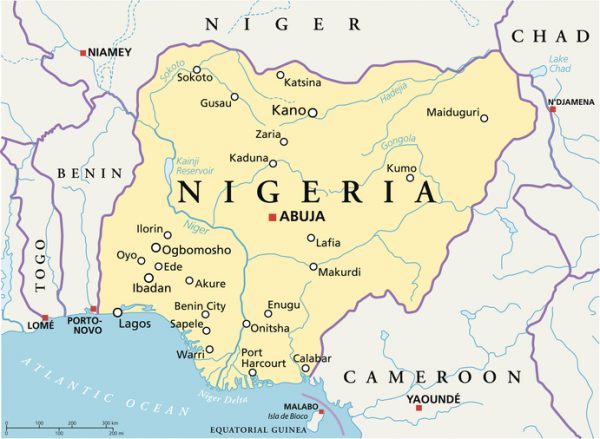
To validate the new approach that Bowden will develop, she sought access to a good-sized cohort of dark-skinned newborns who could participate in a clinical trial. In her preparation, Bowden learned of a clinic in Kano, Nigeria, that was already working with the Vanderbilt Institute for Global Health and Vanderbilt University Medical Center researchers on a related study. With those relationships already in place, Bowden opted to pursue her clinical study there.
Bowden cites two motivations behind this project: to develop technologies that are more appropriate for use in lower resource settings, and to make good health care more accessible. “My postdoctoral research was focused on point-of-care diagnostics for global health applications and was partly funded by the Bill and Melinda Gates Foundation. Since then, I’ve sought ways to do more research in that space,” Bowden said.
“One of the reasons I moved to Vanderbilt was because I wanted to be in a place where I had more freedom to do that work. For me this grant represents the culmination of my long-held desire to conduct research that benefits our global community. I’m very excited about this aspect of this project, which was made possible because of the access to world-class researchers in various departments who can bring their perspectives to a complex problem requiring multiple ways of attack in order to get it done.”
Bowden will be working closely with VUMC faculty, including Dr. Jörn-Hendrik Weitkamp, associate professor of pediatrics and director of patient oriented research, Dr. Martin Were, associate professor of biomedical informatics and medicine, and Bryan Shepherd, professor of biostatistics, to complete this project.
“For me this grant represents the culmination of my long-held desire to conduct research that benefits our global community. I’m very excited about this aspect of this project, which was made possible because of the access to world-class researchers in various departments who can bring their perspectives to a complex problem requiring multiple ways of attack in order to get it done.” – Audrey Bowden
“One of the most important outcomes of this work is in the context of our current social climate around health disparities and other challenges related to health care access. One of the significant controversies most relevant to me is around the failure of some medical processes and technologies to really account for individuals with different skin tones,” Bowden said.
“It has implications for the treatments that people are given or not given. It’s somehow embedded not just in the decisions that the clinicians make, but in the technology itself. As an engineer, I feel that it’s important that we are socially responsible with our designs and that we need to be thoughtful about who is going to be served by this technology. Hence, another outcome of this project is to highlight how important it is to consider all populations who will be affected by the use of this technology in both the technology and study design.”
To this end, Bowden participated in the Boston University School of Public Health conversation, “Towards Antiracist Academic Institutions: Next Steps” in September 2022. She co-authored the comment, “Anti-Black racism in academia and what you can do about it,” which was published in the journal Nature Reviews Materials in August 2021.
