Ibuprofen, naproxen and related non-steroidal anti-inflammatory drugs (NSAIDs) – the subjects of years of study – still have some secrets to reveal about how they work.
Vanderbilt University investigators have discovered surprising new insights into the actions of NSAIDs. Their findings, reported Sept. 25 in Nature Chemical Biology, raise the possibility of developing a new class of inflammation- and pain-fighting medicines.
NSAIDs block the activity of the cyclooxygenase enzymes, COX-1 and COX-2.
“Until about three years ago, we thought we knew everything there was to know about these enzymes and these inhibitors, but we were unaware of some of the details of how they work,” said Lawrence Marnett, director of the Vanderbilt Institute of Chemical Biology and professor of biochemistry, chemistry and pharmacology.
Ibuprofen powerful inhibitor
COX-1 and COX-2 oxygenate (add oxygen to) the lipid arachidonic acid to generate biologically active prostaglandins. Marnett and his team discovered about 10 years ago that COX-2 (but not COX-1) also oxygenates endocannabinoids – naturally occurring analgesic and anti-inflammatory agents that activate cannabinoid receptors (the same receptors that marijuana activates).
The investigators then made a puzzling observation. They found that ibuprofen was a more potent inhibitor of endocannabinoid metabolism compared to arachidonic acid metabolism.
“This was the same drug inhibiting two substrates of the same protein differently,” Marnett said. “We didn’t understand it.”
In the current report, the researchers surveyed a series of different types of NSAIDs for inhibition of COX-2. They included the “mirror-image” versions of ibuprofen, naproxen and flurbiprofen (these drugs come in two different chemical configurations – a “right hand” (R) version and a “left hand” (S) version – over-the-counter ibuprofen is a mixture of both forms). It had previously been assumed that only the S-forms of these NSAIDs (S-profens) were able to inhibit COX-2.
Marnett and colleagues found that the R-profens inhibited endocannabinoid, but not arachidonic acid, oxygenation.

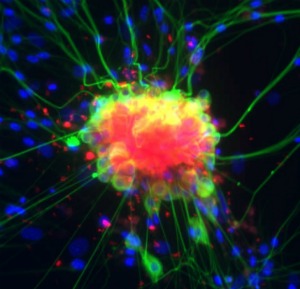
The researchers also determined that R-profens selectively block endocannabinoid metabolism in isolated dorsal root ganglia (neurons and glial cells from the spinal column). They found that treatment of these cultures with an inflammatory stimulus increased expression of COX-2 and stimulated release of arachidonic acid and endocannabinoids, which were oxidized by COX-2. The R-profens inhibited metabolism of the endocannabinoids (and increased their concentrations), but not arachidonic acid.
The findings offer a potential explanation for the reported observation that R-flurbiprofen is analgesic in people and that it inhibits neuropathic pain in a mouse model.
“We’re proposing that R-flurbiprofen is effective in this neuropathic pain setting because it is preventing the metabolism of endocannabinoids by COX-2; so it’s maintaining endocannabinoid tone and that’s the basis for the analgesic activity,” Marnett said.
Better target for analgesia
“It’s exciting because you will only see this effect at sites of inflammation where COX-2 might play a role in depleting endocannabinoids. Selective inhibitors like the R-profens could represent a new way to target analgesia without having the GI, and maybe cardiovascular, side effects of traditional NSAIDs.”
Marnett and his team will pursue this idea by studying in vivo models of neuroinflammation to determine if these drugs – and new compounds they are developing – work to inhibit endocannabinoid oxidation and maintain endocannabinoid tone.
Kelsey Duggan, Daniel Hermanson, Joel Musee, Jeffery Prusakiewicz, Jami Scheib, Bruce Carter, Surajit Banerjee, and John Oates contributed to the studies. The National Institutes of Health (National Institute of General Medical Sciences, National Cancer Institute, and National Institute of Neurological Disorders and Stroke) supported the research.
Marnett is University Professor of Biochemistry and Chemistry, Mary Geddes Stahlman Chair in Cancer Research, and director of the A.B. Hancock Jr. Memorial Laboratory for Cancer Research.