A complex artificial intelligence-powered analysis is being deployed by Jonathan Irish, associate professor of cell and developmental biology and scientific director of the Cancer & Immunology Core, in the race to understand the inner-workings of COVID-19. The tool parses through vast quantities of data to identify extremely rare immune cells that specifically respond to viruses.

Irish’s analysis tool has been in development over the past year to study human immune responses to rhinovirus, a cause of the common cold, in collaboration with the University of Virginia. Upon realizing that the tool could be applied to COVID-19-related research, Irish floated the idea to his colleague at King’s College London where he is a visiting associate professor and honorary senior lecturer. This was the start of an international collaboration between Vanderbilt University and researchers from King’s College London and Guy’s and St Thomas’ NHS Foundation Trust. The group will also collaborate with researchers conducting a similar ongoing study at Princess Margaret Hospital in Canada.
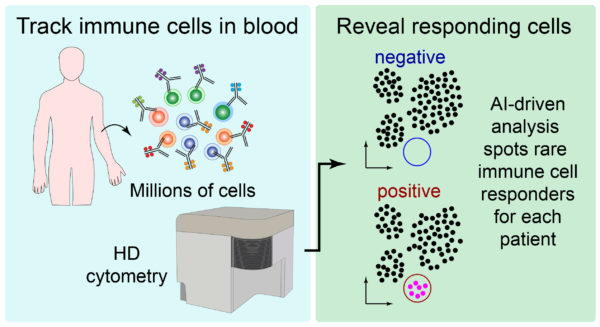
High dimensional (HD) cytometry, a technique that takes measurements of many features of a single blood cell simultaneously, generates so much data that it is difficult for people to parse through. “We think that HD cytometry can be particularly useful in understanding COVID-19,” says Irish. The quickly developing trial will begin treating 19 patients the week of May 31, 2020, and begin collecting samples. Irish’s role will be to analyze and interpret the findings. In rhinovirus, Irish’s tool analyzes pairs of blood cells, one infected and the other not, to compare specific changes to the blood and identify immune cells that are reacting to the virus. But these cells known as antigen-specific T cells are one in a million, literally. “A sample of 10 million blood cells might just contain a couple hundred of these cells. We quickly realized that we could tailor our tool for COVID-19 research because it can pick out these rare cells without any other information,” explains Irish.
The UK-based research team’s trial design is cutting-edge in the sense that it is conducting research while treating patients. This allows the team to see how the trial is working and apply new information to the ongoing trial in real-time. For example, comparing data in patients who need a ventilator with those who do not will provide an unusually clear line of sight into how the immune cells work and what to do next.
The goal of the joint research is to identify which human immune cells are specific to coronavirus infections and distinguish these cells from each person’s immune fingerprint. “Understanding and identifying the types of immune cells that help to fight off the virus could help us optimize vaccine and treatment strategies,” notes Irish.