Vanderbilt University researchers are teaming with peers from two other universities to develop ways to fight disease with light with the promise of minimally invasive, drug-free treatments for cardiac arrhythmia, high blood pressure, asthma, sleep apnea, diarrhea and other diseases.
They’re testing infrared neuromodulation, which targets specific areas of the nervous system and even single nerve cells with light that can stimulate or inhibit electrical signals, altering some bodily functions. Case Western Reserve University School of Medicine is the lead institution on the project, and funding is through a four-year, $9 million grant from the National Institutes of Health.

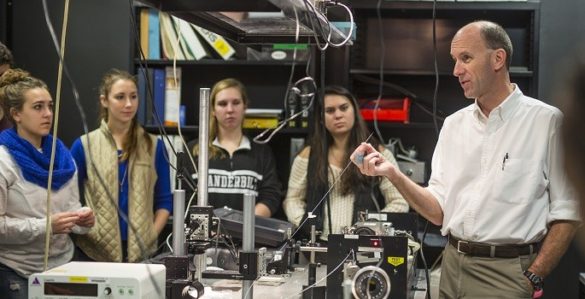
“The potential impact is revolutionary and disruptive,” said E. Duco Jansen, professor of biomedical engineering at Vanderbilt. “We have a lot of engineering, physics and biology work to do before we’re there, and that’s why we’re getting this level of funding.”
Jansen and two other Vanderbilt professors developed the underlying infrared nerve modulation technology for the research: Anita Mahadevan-Jansen, Orrin H. Ingram Professor of Biomedical Engineering, and Peter Konrad, professor of neurological surgery.
Vanderbilt’s role in the current project is unraveling the underlying mechanisms in the nodose ganglion, a cluster of cells that send and receive signals through the vagus nerve to control heart rate, respiration, digestion and several other autonomous functions. Jansen and his group must first figure out which cells are controlling which responses and then how to stimulate one without affecting the others—for instance, lowering blood pressure without inducing asthma.

To do so, they will develop computational models that simulate the body’s responses and also study the interaction of tiny laser pulses with the nerve cells, working towards systems to be implanted in patients
The research is led by Michael W. Jenkins, assistant professor of pediatrics and biomedical engineering at Case Western Reserve University School of Medicine, and also includes researchers from the University of Pittsburgh. The grant is through the NIH’s Stimulating Peripheral Activity to Relieve Conditions program.