One of the realities of cancer is that drugs used to treat it are highly toxic, and effectiveness varies from patient to patient. New “tumor in a dish” technology is poised to assess rapidly how effective specific anticancer cocktails will be on an individual’s cancer before chemotherapy begins.
A team headed by Melissa Skala, assistant professor of biomedical engineering and cancer biology, has developed the technique, which uses fluorescence imaging to monitor the response of three-dimensional chunks of tumors removed from patients and exposed to different anti-cancer drugs.
In an article published last September by the journal Cancer Research, scientists describe applying the technique to the three major forms of breast cancer. They report that the test can detect significant drops in the metabolic activity levels of all three types of tumors within 72 hours when exposed to an effective drug, whereas tumors that were resistant to a drug show no change.
When breast cancer is diagnosed, the drug regimen a patient receives is based primarily on results of a biopsy used to identify the type of tumor. Effectiveness of initial treatment is assessed after two to three months by determining whether tumors are shrinking or continuing to grow.
According to several studies, in more than 100,000 cases each year the breast cancers never respond to standard drugs, either initially or after repeated doses. As a result, 33 to 43 percent of patients must be switched to different drug combinations.
“We hope that our test will significantly improve the odds of survival of breast cancer patients by allowing doctors to identify the most effective but least toxic form of chemotherapy for each individual patient before the treatment begins,” says Skala.
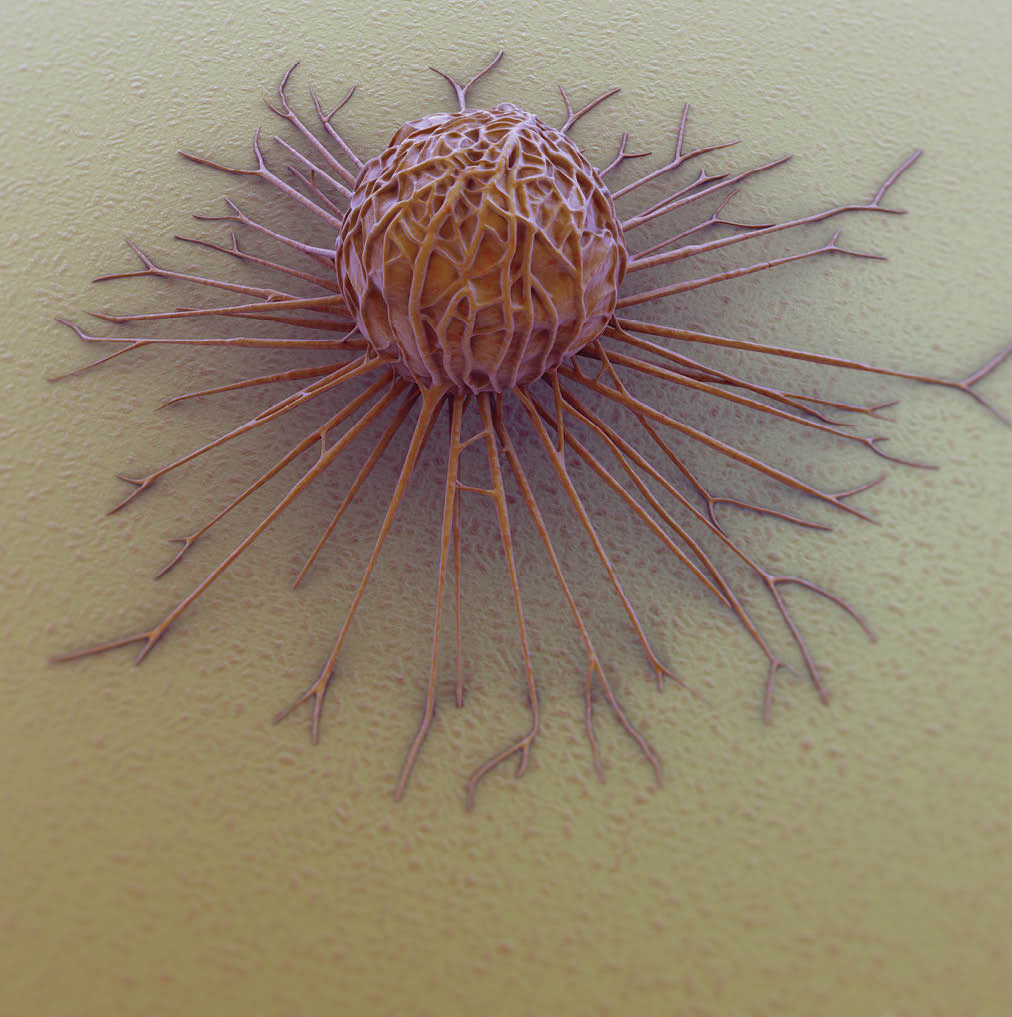
The “tumor in a dish” method begins by taking the cancerous tissue removed during surgery or biopsy, cutting it up into small pieces, and putting the pieces in a special collagen gel. The gel maintains them as “organoids” that retain the three-dimensional structure of the original tumor and include supporting cells from the tumor’s environment.
The traditional method of culturing tumor cells produces a single layer of cells that behave much differently from the original tumor. New methods culture three-dimensional tumor organoids that mimic the behavior of the original tumors, allowing cancer researchers to study how they grow.
“This is the first time the 3-D culturing method has been used to predict the effectiveness of different drugs on tumors from individual patients,” says graduate student Alex Walsh, BE’10, MS’12, who has played a key role in developing the test.
The researchers use a technique called “optical metabolic imaging” to measure the activity level of the organoids. The technique uses a laser tuned to the frequencies that cause two key enzymes in the cells to fluoresce. Measuring the variations in the intensity of the resulting fluorescence provides a “dynamic readout of cellular metabolism,” which is a sensitive biomarker of drug response. Their tests show responses to drug exposures within 24 hours.
“It is cheap and fast and adaptable to high-throughput screening, so it can be used to test dozens of drugs or drug combinations at the same time,” says Skala.
The test also measures responses of all individual cells in the organoid. This is important because tumors are not all alike and some types of tumor cells may respond differently to a specific drug. If a given drug cocktail kills 90 percent of cancer cells but doesn’t affect the remaining 10 percent, resistant tumor cells can cause the tumor to grow back.
“Our test should make it possible to find drug combinations that kill all the cancerous cells in a tumor,” Skala says.
Rebecca Cook, BS’93, assistant professor of cancer biology; Dr. Melinda Sanders, associate professor of pathology, microbiology and immunology; and Dr. Carlos Arteaga, who holds the Donna S. Hall Chair in Breast Cancer, contributed to the research, along with Luigi Aurisicchio from Takis Biotech in Rome and Gennaro Ciliberto from the IRCCS National Cancer Institute in Naples, Italy.
The research was supported by grants from the National Science Foundation, U.S. Department of Defense, National Institutes of Health, National Cancer Institute and Vanderbilt.