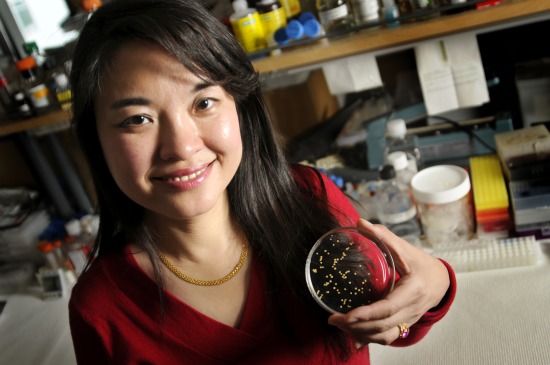
A protein isolated from beneficial bacteria found in yogurt and dairy products could offer a new, oral therapeutic option for inflammatory bowel disorders, suggests a study led by Vanderbilt University Medical Center researcher Fang Yan.
The study, published May 23 in the Journal of Clinical Investigation, shows that the protein, called p40, was effective as an intervention in animal models of colitis (colon inflammation). The investigators demonstrated that the protein supports intestinal epithelial cell growth and function, and reduces inflammatory responses that can cause intestinal cells to die. Importantly, the investigators showed that oral consumption of p40 by mice in a protective delivery system prevents and treats colitis in multiple models of the disease.
Many of the hundreds of bacterial species that live in our gut (known as the “human microbiome”) are helpful to us: they help us digest certain substances, produce vitamins and fight off more dangerous bacteria. But miscommunication between these bacteria and our gut lining can lead to conditions like ulcerative colitis and Crohn’s disease. According to the Centers for Disease Control and Prevention, as many as 1.4 million persons in the United States alone may suffer from these diseases.
One type of helpful bacteria often used in yogurt production and in nutritional supplements, Lactobacillus rhamnosus GG (LGG), has been used in attempts to prevent intestinal disorders such as IBD and diarrhea, as well as other conditions such as dermatitis (skin inflammation). However, results generated using whole bacteria have been mixed.
Yan began studying LGG in 2001 while working in the lab of D. Brent Polk, the former director of the Division of Pediatric Gastroenterology, Hepatology and Nutrition at Vanderbilt.
Exploring probiotics
This research was sparked when a colleague in pediatric infectious diseases asked him, “Is there anything to this probiotic stuff?” said Polk, co-author on the study and currently director of the Saban Research Institute of Children’s Hospital Los Angeles.
“Probiotic bacterial function is not very clear right now,” said Yan, a research associate professor of pediatrics at Vanderbilt.
Polk and Yan showed that LGG prevented epithelial cells from inflammation-induced apoptosis – a kind of cell suicide. They then isolated and characterized two specific proteins secreted by LGG (which they called p75 and p40) responsible for the bacterium’s beneficial effects.
In the current study, Yan investigated the mechanisms by which one of these proteins, p40, prevents and treats colitis.
In cell experiments, Yan and colleagues showed that p40 activates the epidermal growth factor receptor (EGFR), a protein critical for cell survival and growth.
Activation of EGFR protected epithelial cells in two ways: by preventing both apoptosis and inflammation-induced disruption of the “tight junctions” between epithelial cells, which form a barrier to keep toxic substances and pathogens out of the bloodstream.
To test the isolated protein’s effectiveness in animal models of disease, the investigators developed a gel bead system to deliver the protein specifically to the colon while protecting the protein from being degraded by stomach acid and digestive enzymes.
In three different mouse models of intestinal inflammation, they showed that p40 prevented and treated intestinal injury and acute colitis.
Potential therapies
This study is one of the few to identify and use individual molecules from beneficial microbes as potential therapeutics. In clinical applications, Yan says that the isolated protein could provide at least two advantages to using whole bacteria.
“One is bioavailability,” she said. “Even if you eat live bacteria (as in yogurt), that does not mean 100 percent of bacteria will still be alive (and active) in your body.”
Another advantage is safety. Although LGG is generally safe for most people, “in patients with immune deficiency, it could be a problem because it may induce an abnormal immune response,” she noted.
As for the question that initiated these studies, Polk said, “Dr. Yan has answered this with a resounding ‘yes.’”
“It has been my privilege to collaborate with Dr. Yan on this exciting work.”
Polk is also professor and chair of pediatrics and professor of biochemistry and molecular biology at the University of Southern California, and an adjunct professor of pediatrics and cell and developmental biology at Vanderbilt. Other authors on the study were: Hanwei Cao, Timothy Cover, M. Kay Washington, Rupesh Chaturvedi, Yan Shi, Richard Peek, Jr., and Keith Wilson from Vanderbilt; and LinShu Liu, from the U.S. Department of Agriculture.
The research was supported by grants from the National Institute of Diabetes and Digestive and Kidney Disorders, the Crohn’s and Colitis Foundation of America, the National Center for Complementary and Alternative Medicine, the National Cancer Institute and the Department of Veterans Affairs.
Media contact: Craig Boerner
(615) 322-4747