By Amy Wolf
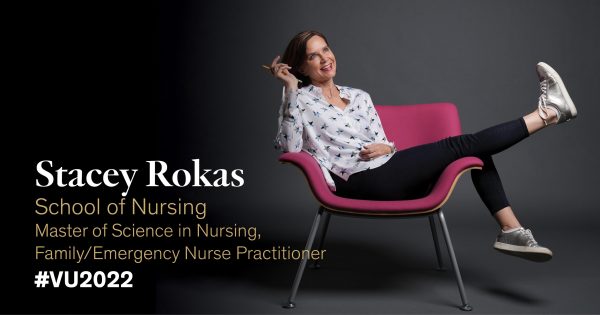
When military nurse Stacey Rokas filled out her application to Vanderbilt University School of Nursing, she was embedded with the U.S. Marines on a training exercise with an international joint force in South Korea. She was the officer in charge of medical care.

“I knew I needed to learn more about emergency medicine to provide better care for the Marine Corps and Navy, but I was wavering on going back to school,” said the nearly 20-year nursing veteran, wife and mother of 10. Rokas almost cancelled her Vanderbilt application, but then fate stepped in.
“In the middle of this remote area, I sat down with a gunnery sergeant, and he had a big Vanderbilt tattoo on his forearm,” she said. “I knew it was a sign.”
Rokas returned from deployment and enrolled in Vanderbilt’s master of science in nursing program to pursue an emergency nurse practitioner specialty. Building on the foundation of the family nurse practitioner specialty, the ENP specialty prepares caregivers for dual certification to practice in diverse emergency care settings.
“Vanderbilt has been at the forefront of this rigorous integrated program,” said Susanna Rudy, instructor of nursing. “With Stacey’s experience and military background, she was an ideal candidate.”
CALLED TO SERVE
In the middle of Rokas’ ENP training, the Navy called her to the front lines again—this time to fight the COVID-19 pandemic in New York City.
“I was deployed with the Navy as a nurse to Elmhurst Hospital in Queens at the height of the pandemic. I had to take care of people on different types of ventilators without staff support, without pharmacy, without respiratory therapy. It was truly a mass casualty situation,” she said.
LIFELINE
That’s when her nursing school instructors became her lifeline to coping with this new and evolving disease.
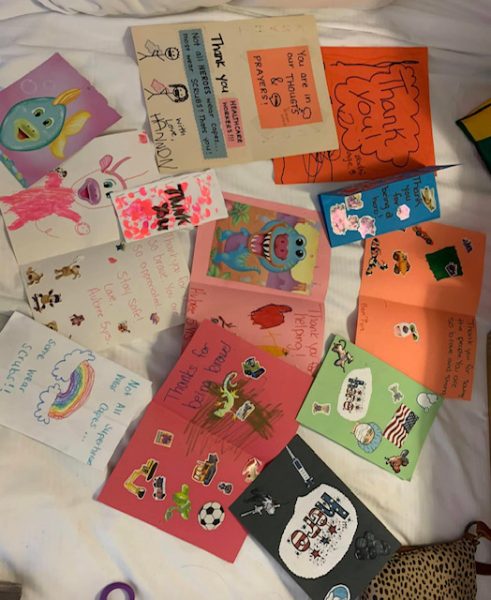
“Vanderbilt became more than just a school. My teachers and my classmates went above and beyond helping me with everything from literal care questions to sending masks and PPE,” she said. “It’s hard to imagine being in a hospital where there’s nothing to clean anything with or the right gear to properly care for patients.”
Rokas knew she desperately needed more training on ventilators, so she turned to Rudy and Jennifer Wilbeck, professor of nursing. They provided moral support as well as practical guidance, like modules on ventilator management and information on evolving emergency care protocols for COVID patients.
“In our program, we teach this transition from emergency medicine to critical care, which was essential during Stacey’s work with critically ill COVID patients,” Rudy said.
Rudy also noted that an ultrasound class that’s standard for the ENP program proved to be highly valuable for Rokas and increased her confidence in using that specialized technology on patients.
RISING TO THE CHALLENGE
Hospitals took note of Rokas’ stellar abilities under pressure.
“Early in the pandemic, on one particular triage call when Stacey was doing clinicals at Baptist Memphis, she was able to identify respiratory distress in a caller over the phone and direct the patient to further emergency care. The leaders of that center were so impressed with her ability to function at that level in such a chaotic environment,” Wilbeck said. “The pandemic showcased in many ways why the ENP role is so critically important in providing front-line health care resources, and how this niche is especially useful in a pandemic.”
Later, while deployed to Queens, Rokas was able to turn to Rudy for support. At the time, Rudy was also in New York City, working on behalf of the Federal Emergency Management Agency to manage out-of-state ambulances that had volunteered to come to the front lines. The two bonded over their shared experiences.
“Not feeling alone in that situation was really everything because I had people to reach out to. It truly showed the character of my teachers and classmates, and I am forever grateful,” Rokas said.
When Rokas returned from COVID duty, she was able to complete Vanderbilt’s rigorous program with new expertise in her nursing toolbox. The program has been so successful that it is now being emulated by other universities.
“Vanderbilt has consistently been at the forefront of emergency nurse practitioner programs since we started ours in 2006. We have a uniquely streamlined educational approach where students first become a family nurse practitioner to provide them primary care expertise. Then we layer on top emergency education, which provides higher-complexity specialty care,” Wilbeck said.
“I love being an emergency nurse, and I wanted a master’s program that challenged me and pushed me beyond what I had learned in my years of practice, which Vanderbilt definitely did!” Rokas said. “But the pandemic taught me that there’s still a lot that we don’t know. So, keep learning and pushing yourself because the minute you think you know it all, you will get a patient who shows you that you need to learn more.”
BRIGHT FUTURE

In the midst of the COVID pandemic and school, Rokas’ family grew. She married her fiancé, Bill, after returning from deployment in New York, creating a blended family with her eight children and his two children. Several of Rokas’ children are currently serving in the military.
The family live near Memphis, Tennessee, where Rokas is currently working in emergency care and remains in the military reserves. She also plans to work with a health care program that aids the homeless population.
“Compassion is what started me on the journey of being a nurse, and it’s essential for everyone in health care,” she said. “Nursing is one of the toughest jobs, but it’s a calling.”










