A fast-paced and comprehensive study has shed new light on how SARS-CoV-2 replicates within host cells. This foundational work may lead to therapeutics that target the replication process, instead of targeting the virus overall.

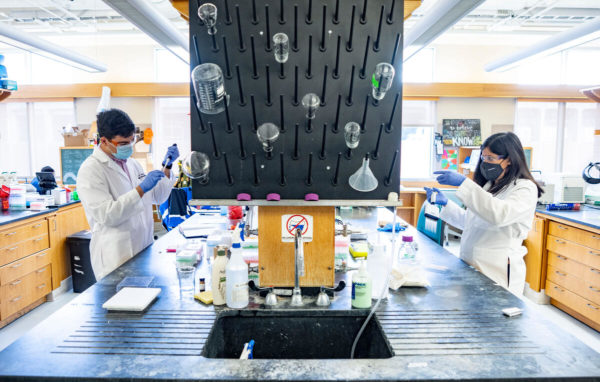
Early in the pandemic, Lars Plate, assistant professor of chemistry and biological sciences, along with graduate students Katherine Almasy, Jonathan Davies and Eli McDonald, investigated the basic molecular mechanisms that give otherwise similar coronaviruses their differing levels of disease severity. Granted special dispensation because of the urgency of the project, the group conducted their research through the shutdown that began in March 2020.
The article, “Comparative multiplexed interactomics of SARS-CoV-2 and homologous coronavirus non-structural proteins identifies unique and shared host-cell dependencies” was published in the journal ACS Infectious Diseases on Dec. 2.
The group examined two nonstructural proteins across three betacoronavirus strains—SARS-CoV-1, SARS-CoV-2 and hCoV-OC43, a strain associated with the common cold—to identify the viruses’ unique and common behaviors among host cells. The proteins were selected for study because they are located near the endoplasmic reticulum and mitochondria, two organelles crucial for cell function. When the virus enters a host cell, it quickly overrides these particular organelles because it needs to control their functions—protein production, immune signaling and metabolism—to survive and multiply, Plate explained.
The researchers used mass spectrometry analysis to simultaneously compare how equivalent proteins from each virus strain interacted with cell components, an approach that made interaction patterns more recognizable.
“The surprising part of the research was in the patterns that we observed, which will influence our future research directions,” Plate said. “By looking at what the viruses have in common, we may well be able to develop host-directed antiviral therapeutics. These therapeutics may be more effective because we do not need to worry about the virus mutating to become drug-resistant.”
One of the most significant patterns the group found was in how the viruses may change calcium signaling within mitochondria-associated endoplasmic reticulum membranes. Among both virus proteins, researchers found interactions with calcium signaling pathways, which can change cell behavior to benefit virus replication. Viral alteration of host cell calcium exchange has been seen in coronaviruses and in Hepatitis C, but not through these proteins nor within the mitochondria, making it an important avenue for further exploration.
The work was funded by National Institutes of Health grants T32 AI112541, T32 GM008554, T32 GM065086, National Science Foundation Graduate Research Fellowship Program grant 1937963, National Institute of General Medical Sciences award R35 GM133552 and funds from Vanderbilt University.