Vanderbilt researcher Ethan Lippmann, assistant professor of chemical and biomolecular engineering, learned in December that he’d won $2.5 million as part of a wider grant from the Chan Zuckerberg Initiative to fund his work on neurodegenerative diseases.
However, it was a family history with Parkinson’s that had originally made Lippmann focus on the topic. “My father-in-law, uncle, and great-uncle, now deceased, all have Parkinson’s disease with varying degrees of severity,” he says. “Seeing their struggles really made the research personal.”
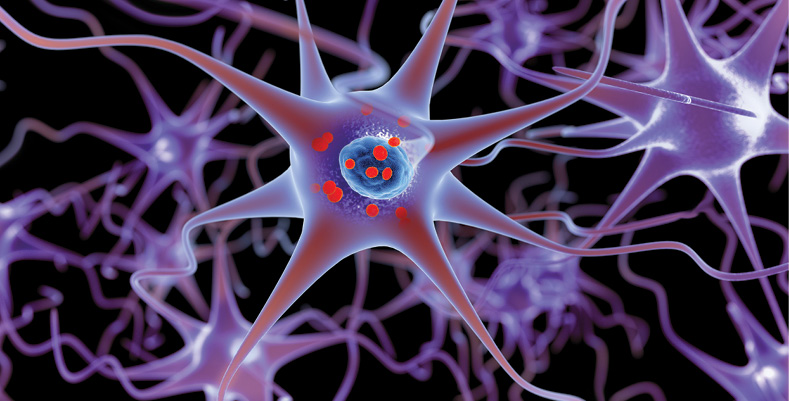
The five-year stipend—funded by the philanthropic organization launched in 2015 by physician Priscilla Chan and her husband, Facebook CEO Mark Zuckerberg—will support Lippmann’s work examining the blood–brain barrier’s role in neurodegenerative diseases such as Parkinson’s and Alzheimer’s. The blood–brain barrier separates most of the circulating blood in the brain from cellular fluid in the central nervous system. Lippmann’s research examines how molecular breakdowns in this barrier contribute to neurodegenerative diseases.
One roadblock to this line of inquiry is that it typically relies on testing animal cells instead of human ones, limiting the insights that could be gleaned about potential causes of neurodegenerative disease related to the blood–brain barrier. Instead, Lippmann has pioneered new models of the central nervous system using self-replicating human stem cells. These stem cells grow plentifully in the lab and can take the form of any cell in the body.
Now, using human stem cells, Lippmann can get a clearer picture of how the blood–brain barrier functions in preventing diseases of the central nervous system. Typically, the barrier serves as a filter that allows beneficial substances to enter the brain while keeping out harmful ones. If the blood–brain barrier malfunctions, some of these toxic substances can infect the brain and cause diseases.
Furthermore, the blood–brain barrier enables the nervous system to regulate various biological mechanisms, such as how much glucose gets into the brain. When the blood–brain barrier malfunctions, these aspects of the brain stop working effectively, and individuals become more susceptible to these diseases.
Studying these interactions, researchers have begun to get a more nuanced understanding of neurodegenerative diseases. “I think the biggest misconception is that there is just one flavor of Alzheimer’s and Parkinson’s when really there are spectrums of the diseases,” Lippmann says. “I also think people associate dementia entirely with Alzheimer’s, when there are lots of different causes of dementia that don’t relate to the core features of Alzheimer’s.”
The next step for Lippmann’s lab will be focused on building representative human-tissue models of the brain that include blood vessels. He plans to use different stem cell sources and engineering methods to achieve this, with the aim of helping reveal the onset and progression of diseases such as Alzheimer’s and Parkinson’s. “I hope that the work done in my lab will ultimately be an important piece of the puzzle,” he says, “for either understanding how the disease progresses or coming up with a novel way of treating it.”
This article was contributed by Gabriella Badmus, a sophomore majoring in communication of science and technology in the College of Arts and Science.