The National Institutes of Health (NIH) has announced that it will award funds to support the next phase of its Tissue Chip for Drug Screening program to improve ways of predicting drug safety and effectiveness. Researchers will collaborate over three years to refine existing 3-D human tissue chips and combine them into an integrated system that can mimic the complex functions of the human body. Led by the National Center for Advancing Translational Sciences (NCATS), the program will support 11 institutions at $17 million in 2014 with additional support over the remaining two years if funds are available.
An interdisciplinary team headed by Gordon A. Cain University Professor John P. Wikswo, Associate Professor of Biological Sciences Donna J. Webb and Associate Professor of Medicine Kevin Niswender will receive $3.2 million to continue development of a neurovascular unit on a chip designed to simulate the unique barriers, such as the blood-brain barrier, that protect the human brain from inflammation, infection, toxic chemicals and other destructive agents carried in the blood. It is not possible to study these critical barriers in an intact brain or in animal models. During the second phase of the program the researchers will assemble an integrated model designed to allow studies of inflammation and metabolism in the brain under conditions like obesity as well as providing an alternative method for studying the brain’s response to promising new drugs as they are being tested for safety and effectiveness.
Fifteen NIH institutes and centers are involved in the coordination of the program. Current funding is being provided by NCATS, the National Institute for Biomedical Imaging and Bioengineering, the National Cancer Institute, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, NIH Common Fund and NIH Office of Research on Women’s Health.
Because these tissue chip systems will closely mimic human function, scientists can probe the tissue chips in ways that they aren’t able to do in people, and the knowledge gained may provide critical clues to disease progression and insights into the development of potential therapeutics.
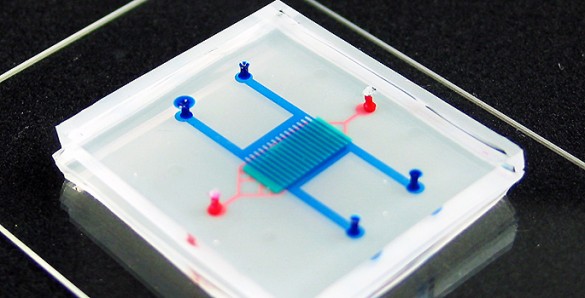
Researchers create human tissue chips using techniques that result in miniature models of living organ tissues on transparent microchips. Ranging in size from a quarter to a house key, the chips are lined with living cells and contain features designed to replicate the complex biological functions of specific organs.
“The development of tissue chips is a remarkable marriage of biology and engineering, and has the potential to transform preclinical testing of candidate treatments, providing valuable tools for biomedical research,” said NIH Director Francis S. Collins.
Approximately 80 percent of candidate drugs fail in human clinical trials because they are found to be unsafe or ineffective. More than 30 percent of promising medications fail due to toxicity, despite promising preclinical studies in animal and cell models. These models can be costly and poor predictors of drug response in humans.
“NCATS aims to get more treatments to more patients more efficiently,” said NCATS Director Christopher P. Austin. “That is exactly why we are supporting the development of human tissue chip technology, which could be revolutionary in providing a faster, more cost-effective way of predicting the failure or success of drugs prior to investing in human clinical trials.”
NIH’s Tissue Chip for Drug Screening initiative is a collaboration between the NIH, Defense Advanced Research Projects Agency (DARPA) and the U.S. Food and Drug Administration. NIH has committed nearly $76 million over the course of the five-year program, which was launched in fiscal year 2012.
In the first two years of the program, researchers developed individual human tissue chips that demonstrated organ functionality, mimicked human biological responses, and generated more accurate data than conventional cell and animal testing methods. Tissue chips include those for the heart, liver, blood-brain barrier, blood vessels, kidney, gastrointestinal system, nervous system, adipose (fat), and models of tumors and metastasis (the spread of cancer). In addition, chips mimicking both male and female reproductive systems will be critical to evaluating differences in response to drug exposure.
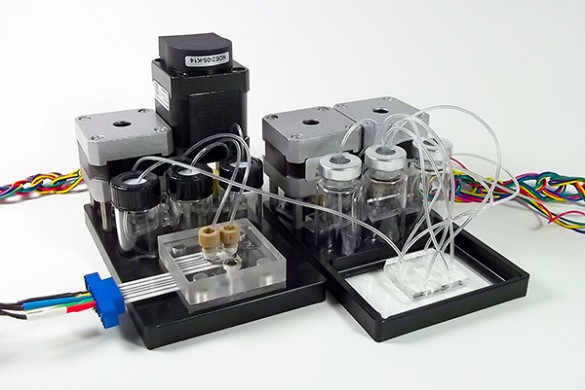
While researchers can use individual chips to study single tissue and organ responses, the integration of chips into a human-like system will enable the real-time measurement of the effects of a drug. The effects will be measured within and across various organs and tissues by which a drug is introduced into the human body, such as the liver and digestive system, as well as the drug’s effectiveness in the organ or tissue it targets, such as the kidney or heart.