Bariatric Surgery’s Metabolic Impact Explored
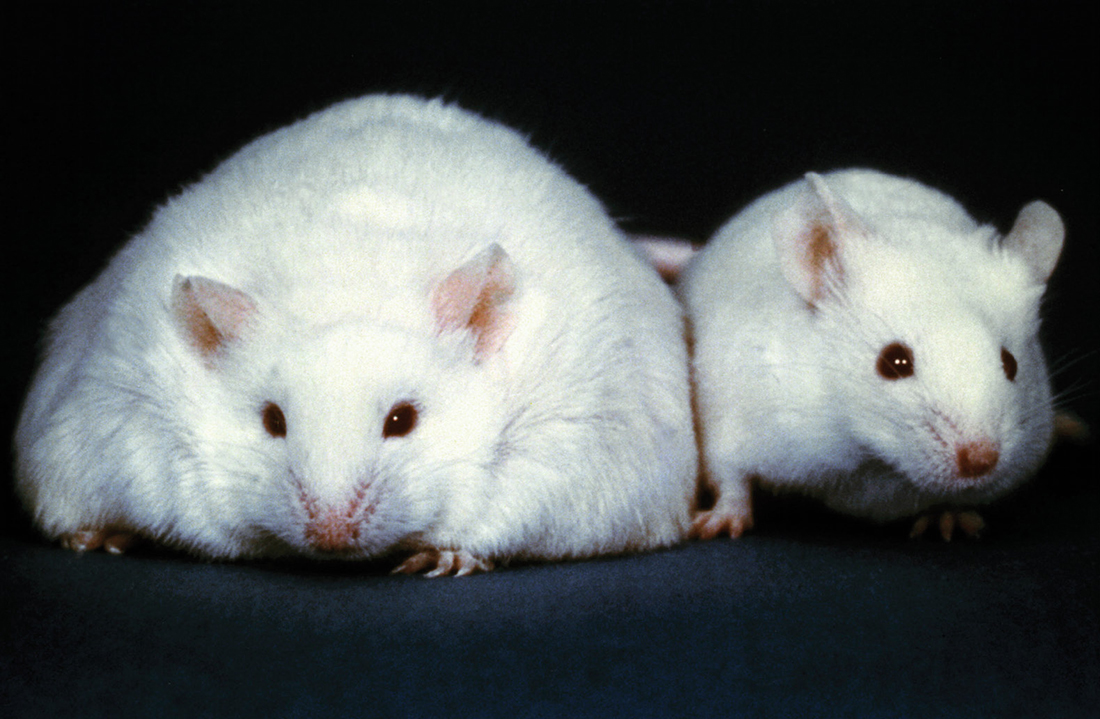
Bariatric surgery is currently the only known effective treatment for severe obesity and type 2 diabetes in humans. Approximately 200,000 bariatric surgeries are performed each year in the United States. Several different procedures are used, but all effectively reduce the size of the stomach.
Recent work has shown that in addition to the reduction in stomach size, many metabolic and hormonal changes likely underlie the beneficial effects of bariatric surgery. Currently, these changes are poorly understood.
After bariatric surgery, 60 to 80 percent of patients with type 2 diabetes, for example, experience a complete resolution of the disease. Remarkably, this often occurs before any significant weight loss and may not be explained by the decrease in food intake alone.
Vanderbilt researchers have received a grant from the National Institutes of Health (NIH) to study a mouse model of the metabolic and hormonal changes caused by bariatric surgery.
Understanding the cellular, molecular and genetic bases for the metabolic changes that result could potentially lead to improved pharmaceutical treatments and surgical techniques, says the study’s principal investigator, Roger Cone, the Joe C. Davis Professor of Biomedical Sciences and chair of the Department of Molecular Physiology and Biophysics.
“The reason it’s important to work in the mouse,” Cone explains, “is that it allows us to use state-of-the-art genetic technologies to understand the mechanism of bariatric surgery.”
Using surgical techniques pioneered by Dr. Dengping Yin, assistant professor of hepatobiliary surgery and liver transplantation, researchers plan to use the mouse model to understand cellular signaling in both the brain and gut, and to determine how this signaling is affected by bariatric surgery.
In addition, they will attempt to determine why bariatric surgery fails to produce significant weight loss in a small number of patients. To identify genes associated with this failure, researchers will use BioVU, Vanderbilt’s DNA databank, which is one of the largest resources of its type in the country.
“The … grant allows us to bring together novel and diverse expertise in central control of feeding, GI function and clinical bariatric surgery,” says David Wasserman, the Annie Mary Lyle Professor of Molecular Physiology and Biophysics and director of the Mouse Metabolic Phenotyping Center.
Other co-investigators are Dr. Naji Abumrad, Dr. Kelli Boyd, Aurelio Galli, Dr. James Goldenring, Dr. Bingshan Li and Owen McGuinness from Vanderbilt, and Dr. Tamas Horvath from Yale University.
The study is supported by a two-year, $1.2 million NIH grant. Other foundational work that led to the grant was made possible by the NIH-supported Vanderbilt Digestive Disease Research Center, Vanderbilt Diabetes Research and Training Center, and by Vanderbilt University.
Learn more about bariatric surgery.