High-density lipoprotein (HDL) is known as “good cholesterol” because elevated levels protect against heart attacks and plaque buildup. However, in some cases HDL may not function properly and may actually accelerate the disease.
Dr. MacRae Linton, who directs the Vanderbilt Lipid Clinic, is principal investigator of a five-year, $11.8 million grant by the National Institutes of Health supporting the search to find out why. The research focuses on three disorders with elevated heart-disease risk: rheumatoid arthritis, chronic kidney disease and familial hypercholesterolemia (FH). FH is a genetic disorder characterized by high levels of low-density lipoprotein (LDL), the “bad” form of cholesterol.
“This is a hot area of debate,” says Linton, the Dr. Stephen J. Schillig Jr. and Mary Schillig Professor of Medicine and professor of pharmacology. But “there’s a lot of evidence to support the idea that HDL cholesterol levels don’t tell the whole story and HDL function is important.”
Linton says that although statins, which lower LDL levels, are the most effective current way to prevent heart attacks, they don’t prevent them all. HDL “dysfunction” may contribute to this “residual” risk. In fact, more heart attacks are associated with low HDL levels than with high LDL levels.
HDL normally takes excess cholesterol from the tissues and delivers it to the liver to be disposed of. But HDL also has anti-inflammatory, antioxidant and antithrombotic functions, Linton says. HDL dysfunction in any of these areas may help explain why some people have heart attacks and strokes even when their LDL levels are normal. “If you could identify the mechanisms causing HDL dysfunction,” he says, “you might be able to go to the next step and design new therapies to prevent heart attacks.”
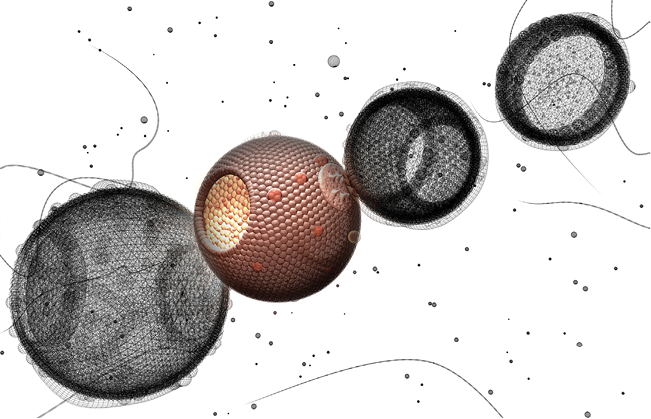
It turns out that HDL carries many different biologically active substances in the blood. One of the major ideas being explored is that the cargo carried by HDL influences its function.
The work also includes grant subprojects led by Dr. L. Jackson Roberts II and Dr. Valentina Kon, working with Sean Davies, C. Michael Stein, Kasey Vickers, Patricia Yancey and colleagues.
Roberts, the William Stokes Professor of Experimental Therapeutics and professor of pharmacology and medicine, is leading a study of isoprostanes, chemical markers of oxidative stress that he and the late Dr. Jason Morrow, BA’79, discovered in 1990.
Kon, professor of pediatrics, is exploring a possible link between HDL function and increased cardiovascular risk in patients with chronic kidney disease. Kon and co-workers recently reported that HDL from end-stage renal-disease patients on hemodialysis was dramatically less effective than normal HDL in accepting cholesterol from macrophages for disposal.
“Patients on dialysis [are] really the only group of high-risk patients where statins have not been able to show a benefit in terms of reducing cardiovascular events,” says Linton. “We think dysfunctional HDL may be an important part of their increased risk.”
Linton is examining factors besides high LDL that may increase heart-disease risk in patients with FH. The anti-inflammatory function of HDL seems to be impaired in patients with the most severe form of the disease.
With Vickers, assistant professor of medicine and of molecular physiology and biophysics, Linton also is investigating the possible role of microRNA in HDL dysfunction. MicroRNAs, which regulate gene expression, are transported in blood by HDL. A goal of the project is to investigate the role of microRNAs on HDL function in FH as well as chronic kidney disease and rheumatoid arthritis.