By Andrew Faught
Along with the blast of arctic air that put much of the U.S. into a deep freeze at the start of 2018, the new year also ushered in one of the most widespread—and deadly—flu seasons in recent memory.
One of the reasons for such misery arose because this year’s flu shot proved particularly ineffective against the H3N2 strain affecting most of those who fell ill. While this latest scourge pales in comparison to the 1918 flu pandemic that killed as many as 50 million people a century ago, it does highlight the dilemma scientists face each year as they try to guess far in advance which strains to guard against with an immunization.
Dr. James Crowe, director of the Vanderbilt Vaccine Center, hopes to solve this problem by eliminating the guesswork altogether.
A renowned microbiologist and Ann Scott Carell Professor, Crowe is leading efforts to decipher the human immunome, a vast set of genes and molecular structures critical to fighting disease. Understanding those mechanics could lead to the development of a universal flu vaccine. No guessing required.
If Crowe and his colleagues succeed, it would likely be one of this century’s most important medical breakthroughs. The findings also could lead to new advances for treating more lethal diseases like Zika, Ebola and HIV.
“There’s so much optimism and buzz in the flu community about the ability to do this,” says Crowe, who was selected last fall to lead the Universal Influenza Vaccine Initiative, an effort to halt a health epidemic that kills 250,000 to 500,000 people around the globe each year.
“Most vaccines are difficult, and flu is one of the more challenging to make,” he says. “But five years ago no one even talked about [a universal vaccine]. Now everyone in the flu community thinks it’s possible.”
The immunome initiative is sponsored by the Human Vaccines Project, a public–private partnership of academic research centers, industry, nonprofits and government agencies working to develop “next-generation” vaccines and immunotherapies.
For now Americans must rely on annual vaccines that are anywhere from 10 to 60 percent effective and are typically created six months before flu season starts. But because the flu virus is prone to mutations, efficacy can be spotty from year to year.
“Sometimes by the time we have the vaccine, we know the guess wasn’t very good,” says Crowe, who also is a professor of pathology, microbiology and immunology. “A lot of smart people use supercomputing and modeling to predict where the flu is going to go every year, but in the end it’s still a guess.”
Despite the flu shot’s limitations, Crowe urges people to get the immunization. That sentiment is echoed by Dr. William Schaffner—Vanderbilt’s widely quoted infectious disease expert and professor of medicine and health policy—saying the influenza outbreak this year is at “the severe end of the spectrum.” Both Schaffner and Crowe say the current vaccine still blunts the flu’s worst symptoms and helps patients avoid deadly complications such as pneumonia and dehydration.
“I get my shot every year, for sure,” Crowe says. But if he gets his way, that’s an annual ritual whose days are numbered.
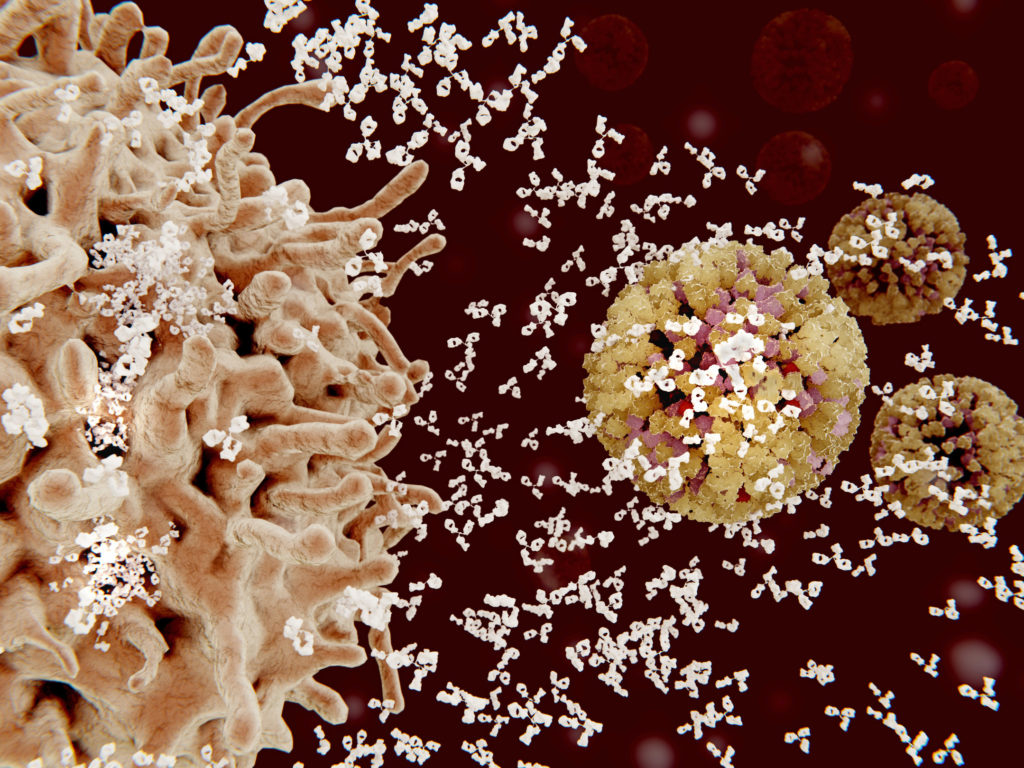
Using new technologies, including artificial intelligence, scientists have discovered previously unknown antibodies—as well as characteristics about the flu virus itself—that offer tantalizing clues about how to develop a universally effective vaccine.
One piece of the puzzle lies in recently discovered proteins in viruses that have remained mostly unchanged for decades. “The discovery of these sites of vulnerability has given everyone optimism,” Crowe says. “The trick, we think, is to find small places on the virus that are not allowed to change.”
Scientists believe that by mimicking these stable portions of the flu virus, they can stimulate production of a rare type of antibody that fights all forms of the influenza virus. But achieving that is akin to finding its Achilles’ heel, says Wayne Koff, president and CEO of the Human Vaccines Project, adding that “people realized there was a gap, a lack of understanding, of the human immune system.”
HUNTING ANTIBODIES
Crowe launched his research efforts last year by harvesting white blood cells, the body’s foot soldiers in the fight against infection. He recruited three healthy volunteers to undergo a procedure known as leukapheresis in which white blood cells are filtered out and then analyzed. “We do a lot of computer work just to figure out what is going on in there,” Crowe says of the procedure.
The study will expand to include 100 volunteers, who will provide baseline data. From there Crowe hopes to inoculate more than 1,000 people with licensed and experimental vaccines. The results will help guide the next generation of vaccine development.
Crowe will use all those white blood cells—about 40 billion from each leukapheresis procedure—to build a comprehensive “parts list” of the immune system.
“Understanding how we respond to influenza virus infection is a critical piece of the puzzle,” says Richard Webby, director of the World Health Organization Collaborating Center for Studies on the Ecology of Influenza in Animals and Birds at St. Jude Children’s Research Hospital in Memphis, Tennessee. “Once we have that, we can start to design our vaccine strategies.”
When attacked by the flu, the human body creates antibodies to fight the illness to varying degrees of success. In a best-case scenario, the virus dies when antibodies adhere to proteins on the surface of the virus. Crowe says a kind of master key of antibodies may exist that could aid in designing a universal flu vaccine.
“Hidden within the [immune] response, there appear to be some rare antibodies that really do have the capability of recognizing all flus,” he says. “The problem is, they’re rare and they’re low in number. Under natural circumstances there aren’t enough of them to really protect us against all flus.
“The idea is to increase the frequency of those rare antibodies, and then they would do the job.”
The goals for a vaccine are modest for now. Rather than a shot each year, “if we could push it out to every three to five years, that would be a good first step,” Crowe says. “Getting a vaccine you only needed every five or 10 years would be the ultimate goal.”
He’s also studying people infected with influenza, hoping to identify more antibodies that can neutralize the virus.
Crowe notes his work is still very much in its infancy. The Human Immunome Program is expected to yield 100 billion times more data than the Human Genome Project. That was a 15-year effort to sequence DNA found in human cells. Sequencing DNA has helped researchers identify genetic mutations and, as one result, tailor treatments for cancer patients. There are similar hopes for the human immunome work.
AVOIDING THE NEXT PANDEMIC
Crowe’s interest in the field stems from his previous work as a pediatrician in sub-Saharan Africa, where infectious diseases are rampant. “Ultimately, I could treat only about 80 people per day, and I sort of dreamed that if we could come up with vaccines that would prevent these things, we could prevent millions of illnesses,” he says. “That’s how it came about.”
He earned his medical degree from the University of North Carolina at Chapel Hill, then received five years of postdoctoral training in the laboratory of infectious diseases at the National Institutes of Health. After completing infectious diseases fellowship training in 1996 at Vanderbilt, Crowe has run an independent laboratory on campus ever since.
An ultra-distance runner in his free time, Crowe is a self-proclaimed daydreamer, pondering the mysteries of his work with every foot fall. The race is long; the finish line is distant. Some vaccines, he says, have taken up to 50 years to develop.
“I don’t want to oversell how far along we are,” he says. “Whether we can reduce these ideas for universal long-lived flu vaccines to practice remains to be seen. It likely will take a decade or so before we can really be sure we have vaccines that work in humans.”
Nonetheless, the Human Vaccines Project cast its lot with Crowe for some important reasons.
“He’s one of those guys who has the ability to think outside the box and have a big vision,” Koff says. “At the same time, he’s detail-oriented and can understand the nuances of science.”
This year Crowe will launch a series of influenza vaccine clinical trials in globally diverse populations. Blood and tissue analysis will then be studied by research institutions that include the University of California, San Diego; The Scripps Research Institute; La Jolla Institute for Allergy and Immunology; the J. Craig Venter Institute; the University of British Columbia; and Lawrence Livermore National Laboratory.
Flu pandemics, meanwhile, are potentially sleeping giants. Besides 1918, less devastating pandemics occurred in 1957, 1968 and 2009. But no one is discounting the potential for a pandemic on par with—or worse than—what happened a century ago.
Population health researchers say a flu pandemic today could kill more than 62 million people, a total higher than all other causes of death combined in any given year. “We didn’t have airplanes [that contribute to disease spread] in 1918,” Koff says. “All the experts in the field are convinced that it’s not a matter of if; it’s really a matter of when. That has led to a lot of interest in the development of a universal influenza vaccine.”
The Human Vaccines Project was developed as the medical community realized it wasn’t making progress quickly enough to conquer complex diseases such as HIV, malaria and tuberculosis, says Koff. Advances in biomedical, computational and engineering sciences have created new understandings of the disease, he adds.
“We really weren’t able, until the last decade or so, even to begin thinking about the human immune system in a serious way because we didn’t have the tools,” Koff says. “This has huge implications for the future of public health, for global health—and Jim’s lab is right in the middle of it.”
Despite the progress, a universal vaccine likely won’t come easy.
Unlike diseases such as smallpox, which affect only humans (thus making eradication of the disease a simpler proposition), influenza never will be eliminated, Crowe cautions. It maintains an “environmental reservoir” in bird and swine species, which readily transmit viruses to humans.
“This has huge implications for the future of public health, for global health—and Jim’s lab is right in the middle of it.”
“When we talk about a universal flu vaccine, we’re just trying to prevent disease in people, not eradicate the disease from the planet forever,” Crowe says. “That’s really the idea.”
Then there’s the sheer complexity of the virus itself. Gazing at an influenza specimen under the microscope, Crowe can’t help but be impressed.
“We look at the atomic resolution images of the virus, and the three-dimensional structures are very complex and beautiful,” he says. “They also have to accomplish a lot of functions. The virus must attach to your cells, change like a switchblade and inject itself into your cell, pick itself apart, make more, put itself back together, and then get out and fold itself back up. How something that’s not actually living can do all that is really impressive.
“Human beings,” Crowe adds, “don’t have enough brain power to create such a particle.”
But we might just be able to outwit its deadliest weapons.
Andrew Faught is a freelance writer based in Fresno, California, and has written widely about issues and ideas in higher education. He earned his degree in journalism at Arizona State University.
Historic Flu Pandemics: Deaths from the flu
 1918 [H1N1]
1918 [H1N1]
Estimated to have infected 500 million people worldwide—a third of the global population—and resulting in the deaths of 20 million to 50 million, the 1918 flu pandemic remains one of the most devastating infectious disease outbreaks. According to the U.S. Centers for Disease Control and Prevention, the virus is thought to have avian origins, although scientists have never determined the properties that made the strain so devastating. The disease’s reach was exacerbated because no vaccine or pharmaceutical treatments existed—only isolation and good personal hygiene.
 1957 [H2N2]
1957 [H2N2]
Another avian-based influenza was first reported in Singapore in February and then in Hong Kong in April. By summer the outbreak had reached coastal cities throughout the U.S. The CDC estimates it caused 1.1 million deaths globally and 116,000 in the U.S.
 1968 [H3N2]
1968 [H3N2]
This strain of flu, which continues to circulate worldwide as seasonal influenza A virus, struck a fatal blow primarily to patients over 65 years old. The estimated number of deaths reported was 1 million worldwide and 100,000 in the U.S.
 2009 [H1N1]
2009 [H1N1]
A new strain of the H1N1 virus emerged in spring throughout the U.S., spreading quickly around the world. Nicknamed the Swine Flu, the virus contained a unique combination of influenza genes not previously identified in humans or animals. It attacked younger patients—those under the age of 60, who perhaps had never been exposed previously to any form of the H1N1 virus. The CDC estimated more than 12,000 people in the U.S. died from the strain, and between 151,700 and 575,400 people died worldwide.