Collaboration between a mechanical engineer at Vanderbilt University and a pulmonologist at Vanderbilt University Medical Center (VUMC) has resulted in a National Institutes of Health (NIH) R01 grant that will be used to develop a steerable robotic needle to safely biopsy hard-to-reach lung nodules.
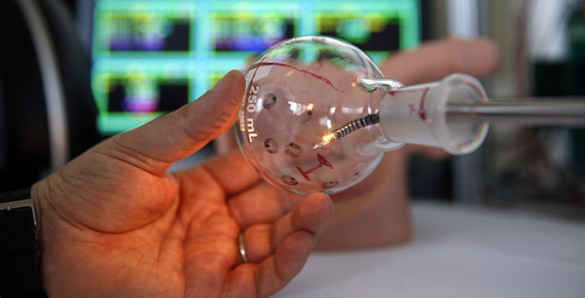
Robert Webster, Ph.D., began to design a beveled, steerable tip needle in 2004 while in graduate school that could help pulmonologists more accurately reach sites in the peripheral lung to biopsy them.
“We were just doing things in blocks of gelatin to see if we could get steerable needles to go where we wanted them to go. At the time, we had no idea that the lung was where this technology would be most useful for doctors — we were thinking about applications in the prostate and liver,” said Webster, associate professor of Mechanical Engineering. “Realizing the amazing potential of steerable needles in the lung was a breakthrough we made in collaboration with Ron Alterovitz and Rick Feins at UNC through an NIH R21 project that concluded a year ago.”
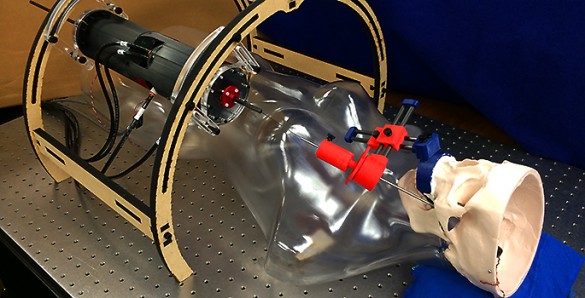
That design laid the initial groundwork for a robotic bronchoscopic delivery system and confirmed that steerable needles work in the lung and could be valuable in retrieving tissue for biopsy. However, Webster needed a clinical collaborator to help advance the system from a crude lab prototype to a real-world medical device usable in the operating room.
Enter Fabien Maldonado, M.D., who joined VUMC in July 2015 from the Mayo Clinic. He is an interventional pulmonologist who commonly uses bronchoscopy as a minimally invasive way to diagnose and treat lung diseases. He reached out to Webster on the recommendation of a colleague to see if they could collaborate on a novel approach.
“We started talking about his research that covers a variety of fields, but specifically the field of lung cancer, which is a huge part of my practice and a huge health care issue,” said Maldonado, assistant professor of Medicine.
“It was not until Fabien came to Vanderbilt and I started talking to him that I finally had someone who could give me the clinical insight I needed in order to make this system work the way it needed to work,” Webster added. “That was the missing piece for me. That has led now to really good proposals and lots of different projects we are working on.”
Webster went on to note that the collaboration was dramatically accelerated by financial support from the Vanderbilt Institute in Surgery and Engineering (VISE).
“We are deeply indebted to VISE for a seed grant that helped us gather preliminary data for NIH proposals, as well as provided a Physician-in-Residence grant that enabled Fabien to spend a day a week in the research lab. This kind of support is just not available at other universities,” Webster said. “Dedicated research time for physicians like Fabien has been the key to accelerating NIH proposals that otherwise would have taken years to mature …if they ever did at all.”
Ron Alterovitz, Ph.D., associate professor in the Department of Computer Science at the University of North Carolina-Chapel Hill, is the principal investigator, with Maldonado and Webster as co-investigators.
Together the team has designed a system that will reach suspicious nodules by deploying a steerable needle from a bronchoscope’s tip. The need for better biopsy approaches is motivated by the fact that lung cancer kills more than 150,000 Americans each year and that survival depends on early diagnosis, which requires biopsy to be definitive.
Current approaches make accurate biopsy challenging or impossible for many nodules. The new system will harness the capabilities of a new class of steerable needles to extend the range of bronchoscopes and reliably and safely access nodules throughout the lung, including in the peripheral zone, Maldonado said.
“It will be technically innovative in that it will combine three types of continuum devices that have not previously been unified, will integrate biopsy collection with a bevel tip steerable needle for the first time ever, and will provide a novel physician interface for visualizing and controlling steerable needles in the lung,” Webster said.