Biomarker tests that help determine which patients may benefit from molecularly targeted therapies need better evidence and oversight to improve their effectiveness and availability, according to a study by the Institute of Medicine (IOM) of the National Academies of Sciences, Engineering, and Medicine.
The study authors said the tests are not being uniformly adopted into clinical practice because of a lack of common evidentiary standards necessary for regulatory, reimbursement and treatment decisions.
Harold L. (Hal) Moses, M.D., Ingram Professor of Cancer Research, chair of the Department of Cancer Biology and Director Emeritus of Vanderbilt-Ingram Cancer Center, served as chair of the national committee that produced the study.
“The timely development of biomarker tests and associated therapies is critical to realizing the full potential of ‘precision medicine,’” Moses said. “Our report lays out a strategy to ensure that patients have access to effective tests and treatments that are based on solid evidence of their ability to improve health outcomes.”
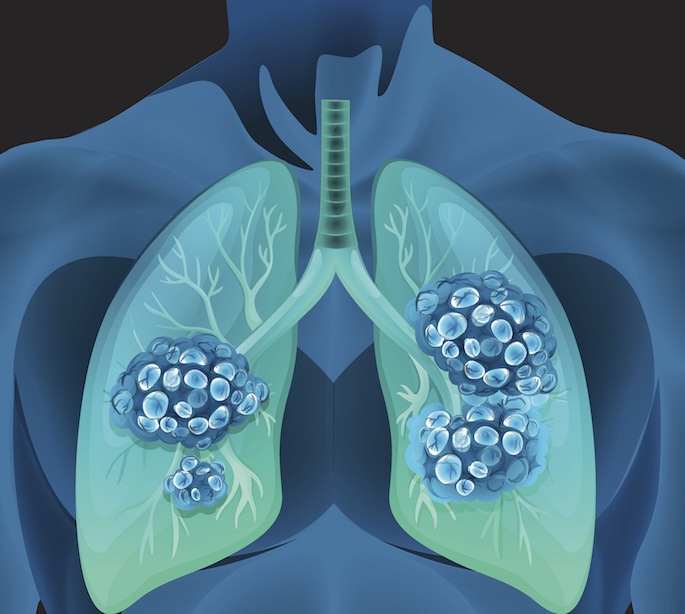
Biomarker tests for molecularly targeted therapies identify molecular variations specific to an individual patient. These tests can help determine which patients will or will not be helped by a targeted therapy and which therapies may actually be harmful.
Advances in research over the past 15 years have led to hundreds of molecularly targeted agents entering the drug development pipeline. Numerous biomarker tests have also been developed and marketed, but the committee found that progress has been hampered by regulatory and reimbursement uncertainties, clinical practice challenges and limitations in data collection and analysis.

Moses said the committee identified 10 goals to advance the development and appropriate clinical use of biomarker tests. They recommended the U.S. Department of Health and Human Services help develop a set of common evidentiary standards for the tests. Those standards would help inform regulatory, insurance coverage and reimbursement decisions and could strengthen clinical guidelines about how and when to use the tests in the patient care setting.
The authors also noted that there needs to be a continuous process to track the clinical benefit of specific biomarker tests and associated therapies. Currently, data on biomarker tests and patient outcomes are not collected or shared in a way that helps physicians make informed decisions.
Yu Shyr, Ph.D., the Harold L. Moses Chair in Cancer Research and director of the Vanderbilt Center for Quantitative Sciences and the Vanderbilt Technologies for Advanced Genomics Analysis and Research Design (VANGARD), served as a member of the national committee.
“When traditional health-care-sector data is linked with genetic data, the assimilation of bioinformatics and health care informatics has the potential to uncover genotype-phenotype associations and become a mechanism for data-driven hypotheses and evidence-based medicine. Thus, the inclusion of genetic information can enhance patient care by providing physicians and patients with valuable risk assessments based on familial and genetic profiles,” Shyr said.
The committee recommended that the Centers for Medicare and Medicaid Services (CMS) work with private insurance companies to develop payment models that support ongoing data collection on the tests and associated targeted therapies. Electronic health records and laboratory information systems should be used to facilitate the collection of patient data in real time, including information about tests, treatments and outcomes. A national database should be created to capture these data to help health care providers and patients make evidence-based decisions about tests and treatments.
The group also noted that some patients may face challenges in obtaining access to biomarker tests and therapies because of economic, ethnic, cultural or geographic barriers. The report calls for research on how to provide equitable access for these patients.