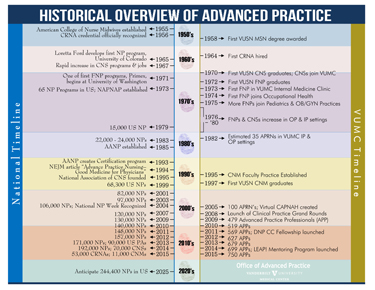
Advanced Practice Registered Nurses (APRNs) have practiced at Vanderbilt University Medical Center for more than 50 years, a landmark achievement for an institution that now has more than 780 APRNs.
More than 100 people celebrated the milestone recently at The Vanderbilt Clinic during the kickoff of the 2015-16 season of Clinical Practice Grand Rounds.
“The Grand Rounds committee orchestrated a tremendous celebration of the past, present and future of Advanced Practice,” said April Kapu, DNP, APRN, associate Nursing Officer and VUMC advanced practice director in the Office of Advanced Practice.
An APRN is someone with a post-graduate education in nursing and a specialized field of knowledge. There are four main categories: Certified Registered Nurse Anesthesiologists, Nurse Practitioners, Certified Nurse Midwives and Clinical Nurse Specialists. Each specialty area is licensed and board certified.
The event’s theme to recognize advanced practice was initially inspired by the American Association of Nurse Practitioner’s national recognition and celebration of the nurse practitioner role, said Janet Myers, DNP, APRN, director of Professional Development. She said the Office of Advanced Practice not only wanted to recognize and celebrate the NP role, but also the other APRN roles.
The celebration featured a panel discussion from three pioneer APRNs at Vanderbilt who recalled their experiences: Leslie Higgins, Ph.D.; Beth Colvin Huff, MSN, N.P.; and Joan King, Ph.D., RNC.
“We are standing on their shoulders because they forged that path for us,” Myers said.
Higgins, who graduated with a Master of Science in Nursing degree in 1975 and took a position in the General Internal Medicine Clinic, recalled those early days.
“I didn’t have a real sense of being anything in the way of a pioneer at that time, but I can remember it was a role that immediately felt right to me,” she said. “I enjoyed having the education and experience to unravel diagnostic puzzles, and to have a group of patients that looked to me as their primary care provider.”
Higgins went on to join the faculty at Belmont University, where she has taught for 21 years and is the Graduate Program director at the Belmont University School of Nursing.
King recalled starting out having a dual appointment as a Clinical Nurse Specialist in the Surgical Intensive Care Unit in August 1975 and as a Vanderbilt University School of Nursing faculty member, barely a decade since the first CRNA was hired at Vanderbilt. She became an Adult Nurse Practitioner, then an Acute Care Nurse Practitioner, and is now professor of Nursing at VUSN and program director for the Adult-Gerontology Acute Care Nurse Practitioner (ACNP) program and maintains an active clinical practice.
King spoke about the importance of APRNs today.
“As APRNs, we expand the quality and the type of care that patients can receive,” she said. “By allowing us to practice to the full extent of our scope of practice, we are able to address patient and family problems quickly and develop appropriate plans of care that help to meet our patients’ needs. In many clinical areas my colleagues are writing prescriptions, doing invasive procedures that either need to be done in a very timely manner or that need to be done as part of the plan of care. All of this allows us to address issues and problems that improve patient care outcome.”
Huff said there were only about 30 APRNs when she was hired in 1980 as a nurse clinician. The term APRN was not yet in use.
“We sought each other out as colleagues and mentors and it was a great support system,” she said. “We helped new APRN hires get introduced around and shared ideas for patient care and staff support. Because we were scattered throughout many areas of the Medical Center, we were also able to use each other as referral sources for patients.”
Huff became an assistant professor in the Department of Obstetrics and Gynecology and worked for many years as the clinical nurse specialist in Gynecologic Oncology.
Roxelyn Baumgartner, M.S., R.N., who has been an APRN since 1982, moderated the panel discussion at the 50th anniversary event. When she started, all the APRNs knew each other. With more than 780 now, she feels like she’s made a difference and that APRNs will continue to make that difference.
“Research and data will drive our evolution and push the boundaries of our practice,” she said. “Health care provided using a team approach to meeting the needs of patients and APRNs is a major presence in this changing paradigm.”
In her remarks, Marilyn Dubree, MSN, R.N., executive chief nursing officer, celebrated the past and future of advanced practice nursing.
“We have long treasured the legacy given to us and felt accountability to honor the work and clinical practice that preceded us,” she said. “The future is bright for your contributions to the ever-evolving health care system. You represent access and care not only across Vanderbilt, but beyond. Your contributions well extend beyond the care you provide to the new knowledge you create, new models of care you implement and the standard you are establishing for APRN practice across the U.S.,” Dubree said.
Finally, in the keynote address of the grand rounds, C. Wright Pinson, MBA, M.D., deputy vice chancellor for Health Affairs and CEO of the Vanderbilt Health System, said, “The APRN role in my opinion has been the hub of care teams for a long time. I have always said they were the glue in the center of the multidisciplinary team. I experienced this in transplantation beginning in the ’80s and continuing throughout my practice career. That is but one example of the importance of APRNs in primary care and multiple specialty care over the last 50 years.
“Going forward, APRNs have a huge role to play in population health. They will increasingly become the backbone of the primary care workforce, given the sheer demand for primary care providers. They will have big roles in care management and care coordination and not just as physician extenders.
“The demand for better provision of mental health services, school health
services, long-term care and palliative care (including end-of-life care) is increasing as well. Care management will become kind of a mini-profession of its own.
“APRNs have key roles to play as team members and leaders for a reformed and better-integrated, patient-centered health care system,” Pinson said.















