In 2013 Vanderbilt University School of Medicine (VUSM) implemented Curriculum 2.0. Tagged as a system of lifelong learning, the deeply integrated curriculum requires flexibility and teamwork on the part of faculty and allows students opportunities to individualize their training.
The new system was divided into three phases of learning — Foundations of Medical Knowledge, Foundations of Clinical Care and Immersion.
This year will be the first time that the full Immersion phase, which comprises the last two years of a medical student’s education, has been rolled out.
In comparison to the prior curriculum in which students fulfilled their core clinical clerkships (Pediatrics, Obstetrics and Gynecology, Neurology, Psychiatry, Medicine and Surgery) during the third year of medical school, Curriculum 2.0 students completed these standardized rotations during their second year of medical school. This change provides students with a longer and more robust post-clerkship experience.
Bill Cutrer, M.D., M.Ed., director of Learning Communities and Curriculum 2.0 Immersion Phase co-director for VUSM, hopes that the program change will allow students an opportunity to fully explore potential career paths while solidifying foundational medical knowledge and skills. Lourdes Estrada, Ph.D., is co-director of the phase.
In other words, students will be able to further build on what they experienced during their clerkships through an in-depth set of courses that use both the clinical setting and, when appropriate, a return to the classroom environment.
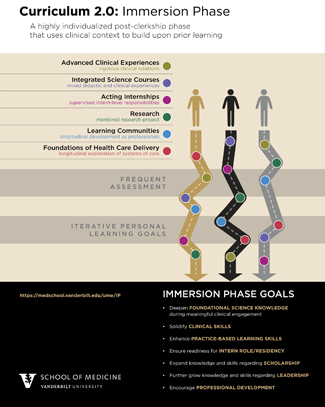
“This is a pretty drastic change from the way we used to do things,” said Cutrer. “Previously, students had one year left of medical school after completing their clerkships. Now students will be exposed to a highly individualized phase that uses their clinical context to build upon their prior learning.
“The Immersion Phase allows students to individualize their schedules to take rotations for exploration and gain a deeper understanding in certain areas,” he said. “While some courses have a more in-depth classroom component, others will be primarily clinical.”
The seven Immersion phase goals are specifically targeted by the three course categories offered:
• Integrated Science Courses (ISCs) target deepening foundational science knowledge during meaningful clinical engagement;
• Advanced Clinical Experiences (ACEs) are rigorous clinical rotations that focus on solidifying clinical skills and practice-based learning skills;
• And the newly designed Acting Internships (AIs) aim to ensure student readiness to function in the intern role as they begin residency training.
The Immersion phase also incorporates teaching of the scientific, ethical, legal and social dimensions of medicine in the clinical care setting.
During a portion of the Immersion phase, students will participate in a three- to six-month mentored research experience, tailored to each student’s research and clinical interests, which will specifically work to expand the students’ knowledge and skills regarding scholarship. The Learning Communities course targets students’ further growth in knowledge and skills regarding leadership, as well as their development as professionals. The Foundations of Health Care Delivery course targets student development as professionals, especially within the areas of health care systems, interprofessional education and population health.
Cutrer said the obvious objective of obtaining a medical degree is a shared goal for the students, but the path will be different for each.
“While each student will take a different road, they will all end up with the same core competency skills and with the addition of key competencies for their individual focus of medicine and interest,” he said.
To ensure a rigorous and robust two-year Immersion phase experience, students will undergo frequent competency-based assessment and personal goal setting, said Kim Lomis, M.D., associate dean for Undergraduate Medical Education.
“Pairing the students’ interests and goals with the review of their performance will allow for a customized Immersion Phase designed to help the student become an outstanding physician,” Lomis said.
The assessment also calls for Curriculum 2.0 students to meet periodically through the Immersion phase with their Portfolio Coaches to review their performance data, set goals for learning in future rotations, and make any necessary revisions to the courses they plan to take.
“The Immersion Phase is critically important for the ultimate success of Curriculum 2.0 and providing individualized pathways through medical school that also allows students to meet all our competency requirements,” said Bonnie Miller, M.D., associate vice chancellor for Health Affairs and senior associate dean for Health Sciences Education. “This also helps us realize our vision of more tightly aligning the training of future physicians with the evolving needs of the health care system.”