Academia and Industry Pool Their Efforts to Speed Discovery of Potent and Personalized New Drugs
By Bill Snyder

Vanderbilt scientists have discovered a series of small molecules that may help unlock the mystery of schizophrenia, a severe mental disorder that can cause disabling hallucinations, delusions and disorganized thinking.
If they can refine the molecules into drug-like compounds, and pass the baton to a drug company for further development, the result could be a new class of drugs significantly more effective than current therapy and with fewer side effects. The work is slow going, and the risk of failure is high. Even if a candidate compound passes the rigorous safety and efficacy testing required of a potential new drug, it may be 2016 before it can be tested extensively in patients, and 2020 before it reaches the market.
But the project, conducted in collaboration with the global biopharmaceutical company AstraZeneca, represents a paradigm shift in the way novel drugs are discovered and developed. The hope is that such partnerships will significantly improve treatment of a host of disorders, from serious infections to cancer and diabetes.
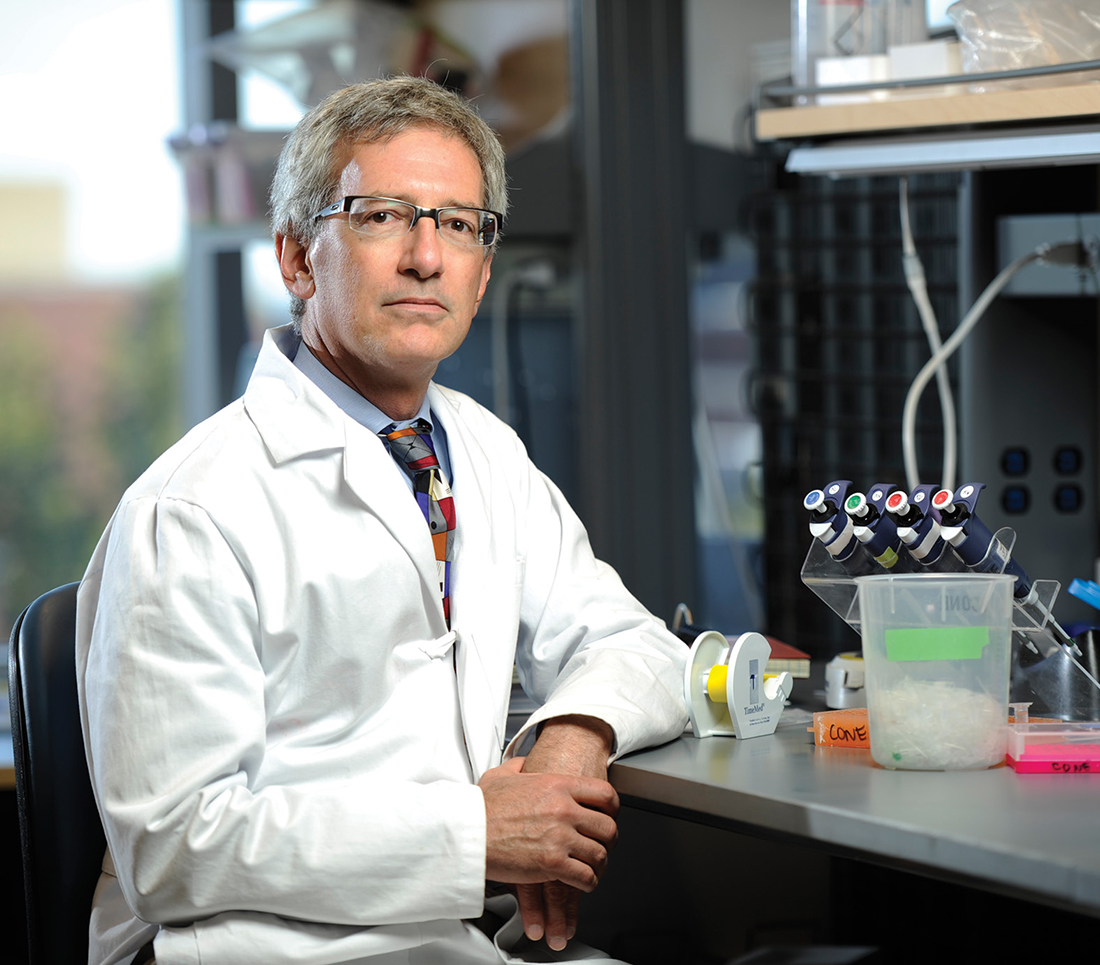
What distinguishes Vanderbilt, says Craig Lindsley, who leads the schizophrenia project, is that drug discovery is run in parallel with basic research—“deep biology”—in an effort to understand the pathophysiology of the disease down to the molecular level.
That research is supported by the university, the National Institutes of Health (NIH), philanthropy and, increasingly, revenues from licensing agreements negotiated by the Vanderbilt Center for Technology Transfer and Commercialization (CTTC).
“If we don’t invest in the basic science, we’re not going to be successful,” says Lindsley, director of medicinal chemistry in the Vanderbilt Center for Neuroscience Drug Discovery. Lindsley is the William K. Warren Jr. Professor of Medicine and a professor of pharmacology and chemistry.
“I feel schizophrenia is the scourge of all illnesses because of its devastating, vulnerable symptoms,” says William K. Warren Jr., chairman emeritus of the Oklahoma-based foundation named for his father. “Other illnesses receive a lot more attention, but we must support ‘deep biology’ research to better understand and treat this horrific illness.”
Schizophrenia affects an estimated one of every 100 adults. Current medications can keep hallucinations and delusions at bay but do little to address other symptoms, including cognitive difficulties and a tendency to withdraw from others. The drugs also cause side effects that can be devastating for patients and family members, including metabolic disorders and significant weight gain.
FREEDOM OF PURSUIT
Shannan’s husband was diagnosed with schizophrenia six years ago. “Some of the medications he’s been on have just made him very foggy and lethargic, sleepy and withdrawn,” she says. “His whole personality is kind of erased.”
 Jerold, who was diagnosed with schizophrenia as a child, is trying to go back to work after 20 years. “I was too sick,” he says. “We are just hoping for new medications to come out so we can feel better about ourselves and have the kind of life that everybody else has.”
Jerold, who was diagnosed with schizophrenia as a child, is trying to go back to work after 20 years. “I was too sick,” he says. “We are just hoping for new medications to come out so we can feel better about ourselves and have the kind of life that everybody else has.”
Jerold and Shannan are two of the many people who have contacted Vanderbilt in response to previous publicity about the AstraZeneca collaboration. Only their first names are used here, with their permission, to protect their privacy.
“Clearly, there are huge unmet clinical needs,” says Mark Duggan, vice president for neuroscience at AstraZeneca.
“That’s why we are continuing to invest in neuroscience but via external scientific partnerships with some of the best groups around the world, including Vanderbilt,” adds John Dunlop, also a vice president of neuroscience at AstraZeneca. “Together we are aiming at getting a compound that could advance into clinical testing.”
The target of the collaboration is the M4 muscarinic acetylcholine receptor, which in the brain binds the neurotransmitter acetylcholine. In animal models the Vanderbilt scientists have shown that “allosteric modulators” of M4 can “ramp up” the receptor’s activity without affecting other signaling pathways. The result is an improvement in cognitive impairments and behavioral disturbances that, in humans, are associated with Alzheimer’s disease as well as schizophrenia.
Craig Lindsley, along with P. Jeffrey Conn, PhD’86—the Lee E. Limbird Professor of Pharmacology, who launched the university’s neuroscience drug-discovery program in 2003—and their colleagues, have pioneered the use of allosteric modulators to adjust the activity of neurotransmitter receptors in the brain. Rather than activating receptor activity directly, these compounds work like dimmer switches in electrical circuits and induce more subtle changes in receptor function than are seen with traditional receptor agonists.
“We do really good basic science on novel targets and novel mechanisms, and we publish in high-profile journals,” says Lindsley. During the past six years, “we’ve published nearly 300 papers and we’ve filed about 290 patents,” he says. The program also trains graduate students and postdoctoral fellows in translational research. “You can’t find that at most universities: the ability to … be trained by industry-knowledgeable scientists.”
So far, every graduate student has gotten his or her first choice of a postdoc position. “If they wanted to go into industry, they’ve all gotten jobs,” Lindsley adds. “We don’t have anyone looking for work.”
“We’re in a sweet spot here,” says Thomas Bridges, PhD’10, a former Vanderbilt graduate student and postdoc who is now part of a dedicated team of scientists assigned full time to the AstraZeneca collaboration. “We can pursue … a deep understanding of our targets. There’s a lot of freedom in it.”
PROGRESS IS FRAGILE
Vanderbilt’s strength in drug discovery grew out of its early commitment to clinical pharmacology, the study of how drugs work in the body.
These efforts weren’t limited to the School of Medicine. The establishment of the Vanderbilt Institute of Chemical Biology (VICB) in 2002 under the direction of Lawrence Marnett, University Professor of Biochemistry and Chemistry and the Mary Geddes Stahlman Professor of Cancer Research, demonstrated the university’s encouragement of cross-campus, multidisciplinary collaborations.
When it comes to translating basic research discoveries into advances in clinical medicine, “chemistry is at the heart of it,” says Marnett. “Chemists make new molecules that become drugs. Chemists develop analytical methods that are at the heart of biomarker development.”
About a fifth of VICB’s 80 faculty investigators have primary appointments in the Department of Chemistry. Several investigators, beginning in 2003 with the arrival of Conn and Brian Bachmann, associate professor of chemistry and biochemistry, were attracted from industry.
Success tends to breed success. Due in part to its drug-discovery effort, Vanderbilt’s ranking in terms of total spending on “chemical R&D” catapulted from 33rd place in 2010 to 12th place in 2011, according to the Dec. 9, 2013, issue of Chemical & Engineering News. Today Vanderbilt has one of the top drug-discovery programs in the country.
Vanderbilt’s ranking in “chemical R&D” catapulted from 33rd place in 2010 to 12th place in 2011. Today Vanderbilt has one of the top drug-discovery programs in the country.
Medicinal chemistry is the stage at which compounds are identified, made and tested for their ability to bind to, and affect the activity of, a target like M4. That’s followed by molecular pharmacology, drug metabolism and pharmacokinetics, and then behavioral pharmacology, to test their potential to become drugs.
|
|
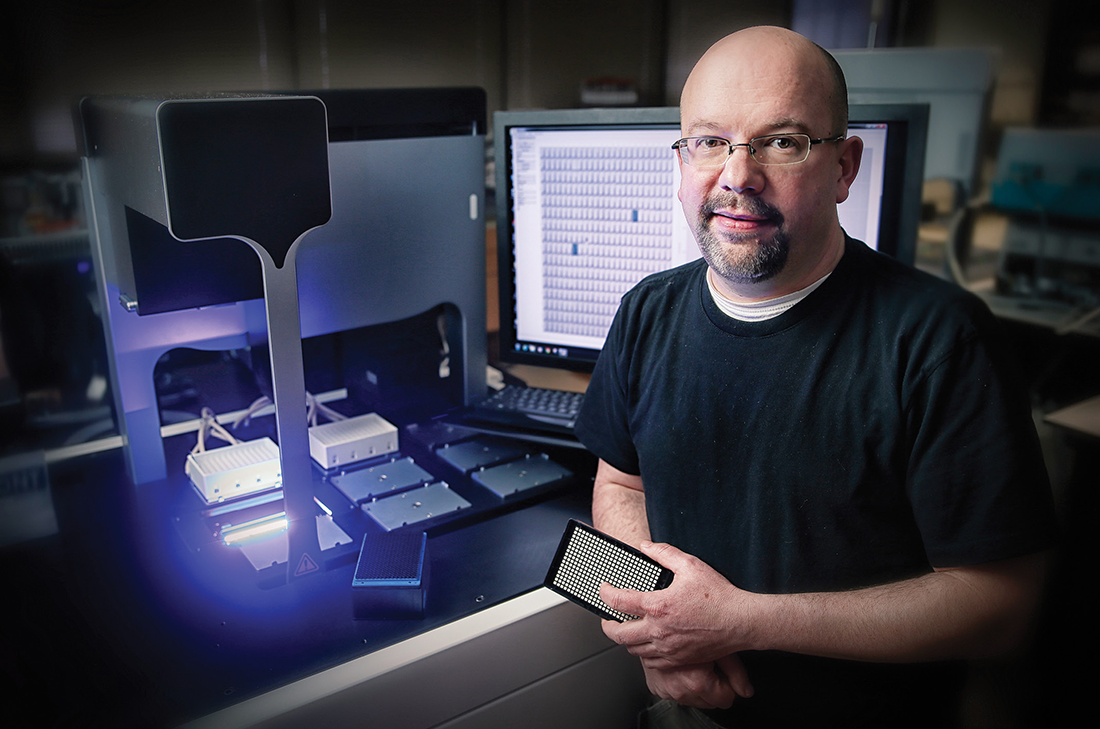
The first stage—identifying drug-like compounds—has been accelerated dramatically in recent years through advances in high-throughput screening (HTS). Vanderbilt’s HTS facility, established by David Weaver in 2005, has a “library” of 190,000 compounds and the ability to test tens of thousands of samples per day.
“One of my basic assumptions is that I don’t understand too much about how the system works,” says Weaver, assistant professor of pharmacology. So he tries to develop “open-minded” assays, designed to let scientists detect unanticipated effects of a potential drug on a drug target, for example.
Fancy screening techniques aren’t enough, of course. Potential drugs must show efficacy and safety in animal models before tested in humans, and many a promising agent has failed when it got to the clinical trial.
The problem with schizophrenia, at least for would-be drug discoverers, is that, like cancer, it is not one disease but many. Its constellation of symptoms, behaviors and cognitive impairments probably results from more than one genetic mutation affecting multiple proteins, receptors and signaling pathways throughout the brain.
That’s why some drugs work in some patients but not in others. If potential new drugs could be “matched” with research subjects most likely to respond to them based on their “genotype” or genetic makeup, the success rate for clinical trials would be much higher, Lindsley says.
“We need the right molecules for the right mechanisms in the right patients,” agrees AstraZeneca’s Dunlop. Thanks to advances in psychiatric genetics, that day is coming, and may arrive within the next decade, he says.
Vanderbilt is well positioned to translate these advances into tangible benefits for patients like Jerold and Shannan’s husband—if it continues to invest in new technologies, facilities and people.
But scientific progress “is a very fragile thing,” says Marnett. “Even though we’ve got a lot of people doing some really exciting things … if the garden isn’t tended, it unravels pretty quickly.”
A former newspaper health care reporter, Bill Snyder is a senior science writer and manager of VUMC Research Communications.