In June, Tommy Schroader was in the crystal blue waters off Grand Cayman Island petting a giant stingray.
Lifelong epilepsy and the risk of seizures had kept him from adventures like this, but after a successful procedure at Vanderbilt University Medical Center last December, he was celebrating six months of being seizure-free.
His wife, Miranda, was with him on the celebratory Caribbean cruise and says they are amazed at how much life has changed, for both of them.
“To see how much it improved our life, the benefits definitely outweigh any risk. We were expecting it would be a good outcome, but never thought it would be this much of a life changer,” she said.
An elementary school physical education teacher in Brighton, Tenn., Schroader, 40, was constantly worried about getting enough rest and staying relaxed because fatigue or stress would make his seizures more frequent. A huge sports fan, he still found time for his beloved St. Louis Cardinals, but had to avoid any activity that would be dangerous during a seizure, like being near water.
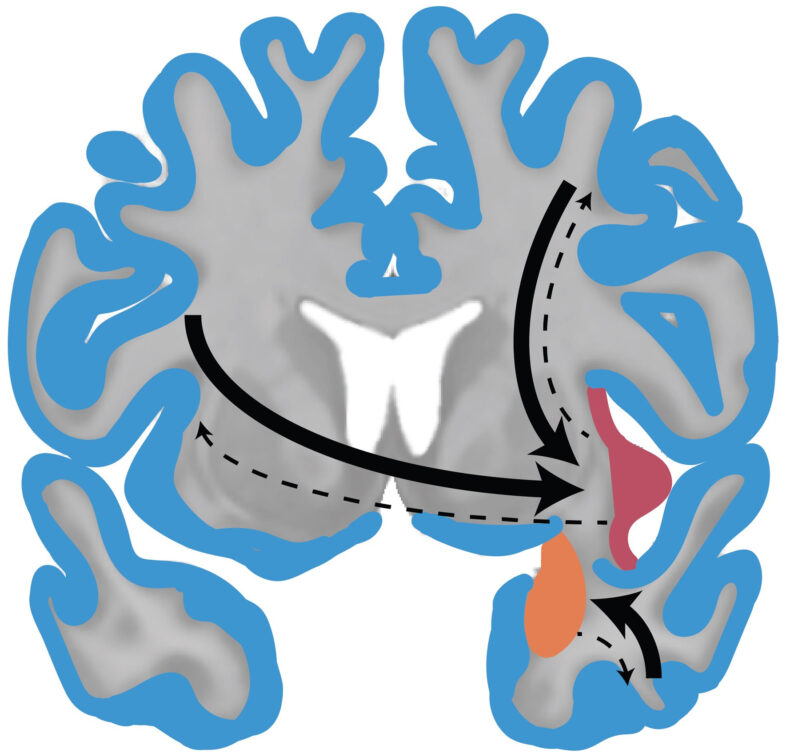
Epilepsy is a neurological condition that disrupts electrical signals in the brain and is characterized by seizures, which can range from a mild staring spell to severe convulsions.
Joseph Neimat, M.D., assistant professor of Neurological Surgery, says epilepsy surgery is “one of the most gratifying treatments in neurosurgery that we provide.”
The surgery involves removing the portion of the brain where the seizures originate, and about 70 percent of patients who have surgery are completely seizure-free. Others have reduced seizures while a small number have no improvement or worsening.
“Epilepsy surgery is often treated like an absolutely last resort surgery, and I think that’s a huge mistake because to date it is the most effective treatment for seizure,” Neimat said. “The recommendation of the National Epilepsy Foundation that we follow is to try three drugs, and if those don’t work an evaluation for surgery is appropriate.”
Schroader had his first seizure at 18 months old, and says he had tried nearly every available medication available to try to control his seizures.
“I’m always aware a seizure is coming on. I can’t talk, I feel dizzy, my head turns side to side,” he said.
As a child, Schroader was cared for at Vanderbilt by Gerald Fenichel, M.D., now retired from leading Pediatric Neurology.
In June 2011, his adult neurologist in Memphis, Ken Henderson, M.D., referred him back to Vanderbilt for a surgical evaluation.
The evaluation, conducted in VUMC’s inpatient epilepsy monitoring unit, puts patients through a battery of tests to determine where the seizures originate and if it is safe to do surgery.
Then the entire team of neurosurgeons, epilepsy specialists, fellows and technicians meets to review data from the tests and discuss how to proceed.
Epilepsy surgery was pioneered in the 1950s, and today Neimat and Peter Konrad, Ph.D., associate professor of Neurological Surgery, perform about 50 procedures per year.
Schroader’s was a relatively straightforward case because his seizures originated in a single area, the hippocampus, a common site. Neimat opted for a minimally invasive surgery to remove just the hippocampus, tissue about the size of the first two knuckles of the pinky finger, using a small incision and microinstruments.
“It lies up against some important stuff — blood vessels that are feeding the brain stem and the optic nerve — but with the minimally invasive approach, it’s an easier surgery and he bounced right back,” Neimat said.
“There is always some risk with surgery, but it is very, very small. And with a 60-70 percent seizure freedom rate, I think the benefits far outweigh the risks.”
In December 2011, after an eight-hour surgery and three days in the hospital, Schroader was home in time for Christmas. 
Six months later, he was swimming with the stingrays.
As he steps down from medication, Neimat said Schroader will continue to see improvements.
“What always surprises me when talking to these patients is not just that the seizures are gone but that their thinking becomes more clear and they say they can do things they were never able to do before — go back to school or start their own business — when before they couldn’t even concentrate enough to balance their own checkbook. It can be a real life-changer.”
Now the Schroaders are in the process of adopting a child.
“That was one of the main reasons I went for it,” Schroader said, “to be the best husband and dad I can be without epilepsy hanging over my head.”