Infants who have higher amounts of the bacterium Lactobacillus present in their nose or upper part of the throat during an acute respiratory syncytial virus (RSV) infection are less likely to develop childhood wheezing later in life, a new Vanderbilt-led Center for Asthma Research study found.
Lactobacillus is a type of “friendly” bacteria that normally live in the digestive, urinary, and genital systems without causing disease.
The study was published in the Journal of Allergy and Clinical Immunology. The latest finding in the research on RSV, one of the most common causes of upper and lower acute respiratory infection in young children worldwide, is important for researchers as they look to create interventions that prevent the development of childhood wheezing illnesses, including asthma.
Childhood wheezing illnesses have commonly been associated with RSV, however, the pathways underlying the association aren’t fully understood.
“These findings provide new insights not only about how RSV infection in infancy may cause wheezing later in life, but also how the normal bacteria that live in and on us may protect us from disease,” said Christian Rosas-Salazar, MD, MPH, one of the study’s first authors and assistant professor of Pediatrics.
The researchers conducted a study of previously healthy, term infants who had laboratory-confirmed RSV acute respiratory infection (ARI).
The infants were enrolled in the INSPIRE (Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure) study — a population-based birth cohort of infants born between June and December, designed so that the first RSV infection during infancy could be studied. Eligible infants were enrolled from collaborating general pediatric practices throughout the Middle Tennessee region.
Researchers collected samples of bacteria from the infants’ noses and upper throats. The infants were followed until age 2, when their wheezing outcomes were assessed. The detection and increased abundance of Lactobacillus in the infants’ noses and throats was consistently higher in infants who did not develop wheezing at 2 years.
With this information, the researchers suggested, “the detection of Lactobacillus in the nasopharynx of RSV-infected infants could be used as a biomarker for the later development of childhood wheezing illnesses.”
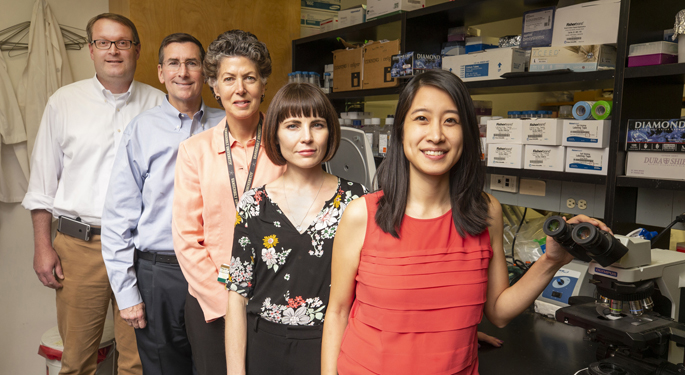
Other Vanderbilt study authors included: Tina Hartert, MD, MPH; Suman Das, PhD; Meghan Shilts, MHS, MS, James Chappell, MD, PhD; Emma Larkin, PhD; Tebeb Gebretsadik, MPH; and R. Stokes Peebles Jr., MD. Study authors from the J. Craig Venter Institute included: Andrey Tovchigrechko, PhD; Rebecca Halpin, MS; and Karen Nelson, PhD. Study authors from Emory University included: Martin Moore, PhD; and Larry Anderson, MD.
The study was funded by the National Institutes of Health (NIH)/National Institute of Allergy and Infectious Diseases, (under award numbers U19AI095227, K24AI77930, HHSN272200900007C, and U19AI110819). Additional funding included: the Vanderbilt Institute for Clinical and Translational Research grant support (under NIH/National Center for Advancing Translational Sciences award numbers UL1 TR000445 and U54RR24975); the Vanderbilt Faculty Research Scholars Program; and the Parker B. Francis Fellowship Program.