For decades the miracle of organ donation has relied on an ice cooler.
Until now.
Vanderbilt University Medical Center is one of nine centers across the United States to participate in the EXPAND Heart Pivotal Trial, which has the potential to change the way donor hearts are preserved and transported to recipients.
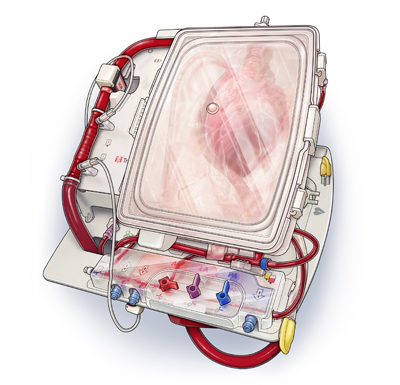
The trial will use a device by TransMedics called the Organ Care System (OCS) to keep the heart beating and metabolically alive during transport from the donor to the recipient. The machine is designed to keep the heart beating outside of the body (ex-vivo).
Currently, surgeons work to transplant a heart within four hours after it has been harvested from the donor’s body. OCS can extend that time frame, allowing the heart to withstand longer periods of time outside of the body.
“Traditionally, transplantation was built upon the premise that we can take an organ out, put it on ice, leave it in this metabolic quiescent state allowing you to transport that organ to the appropriate recipient,” said Ashish Shah, M.D., chair of the Department of Cardiac Surgery and director of Heart Transplant and Mechanical Circulatory Support at Vanderbilt University Medical Center (VUMC).
“Every minute counts during cold ischemic storage, when there is no blood circulation. After three hours, the initial heart function can be compromised. It appears that the longer a heart is on ice the higher the risk that it will be impacted.
“But what if we removed the time element?” asked Shah. “The concept of leaving the organ beating, working and accessible is the next step in heart transplantation. The possibilities are wide open.”
OCS is a portable perfusion and monitoring console that pumps warm, oxygenated, nutrient-enriched donor blood into the heart to optimize the function and also allows for continuous clinical evaluation by the medical team. The console is equipped with a wireless monitor, disposable perfusion module and a heart solution set to keep the heart in a living state until time for transplantation.
While the use of standard cold storage for preservation and transportation reduces the metabolic demands of the heart as well as slows the rate damage, there is no blood circulation and subsequently, some damage does occur, Shah said.
OCS has the ability to increase the amount of time that a heart can be maintained outside the body in a condition suitable for transplantation, providing surgeons the opportunity to assess the heart’s function outside the body and allow for resuscitation, which could potentially improve function after removal from the donor.
In earlier trials, called PROCEED and PROCEED II, OCS outcomes were similar to outcomes of hearts preserved with standard cold storage.
Now the EXPAND trial will allow centers to further broaden the device’s use to include donor hearts that did not meet the current standard criteria for donation. Hearts falling into that category include those that would require longer than four hours on ice, hearts that have reduced function, as well as hearts with coronary artery disease.
Vanderbilt, the only heart transplant program in the region using the novel perfusion technique, expects to begin the trial later this year with its first recipient.
Other EXPAND trial centers include Cedars-Sinai Medical Center, University of California Medical Center, Los Angeles, University of Michigan, Duke Medical Center, University of Washington, Spectrum Health, Grand Rapids, University of Minnesota Medical Center and Massachusetts General Hospital.
“The idea is to expand the donor pool,” said Shah. “Opening up the criteria for heart donors will do two things: get people transplanted faster because the geographical area has increased with the removal of the time constraints; and secondly, it allows us to create new knowledge in this innovative field of organ reconditioning and resuscitation.
“Vanderbilt is uniquely positioned to contribute to this endeavor because of our collaborative scientific and clinical environment. We have the infrastructure to embark on this novel approach to heart transplantations.”
He expects the new technique to revolutionize heart transplantation.
“What if we could use this platform to repair hearts?” asked Shah. “When I look at this technology I am inspired by the extraordinary possibilities of what this holds for the future of transplantation.
“We are putting our intellectual muscle behind this and playing a role in inventing the future instead of following the crowd.”
While OCS is still experimental in the United States, it has been approved for use in other countries.















