Researchers at Vanderbilt University Medical Center (VUMC) have found a way to calm the “genomic storm” that triggers the often-lethal consequences of sepsis.
Sepsis, an exaggerated and overwhelming inflammatory response to various infections, is a leading cause of death in the United States and around the world.
Using a cell-penetrating peptide they developed, the researchers suppressed in an animal model of polymicrobial sepsis the transport of pro-inflammatory transcription factors into the cell’s nucleus. That, in turn, prevented activation of inflammatory pathways and reduced resulting blood vessel damage, respiratory distress, multiple organ failure and death.
Their findings, reported this week in the online journal PLOS ONE, highlight the potential benefit of targeting nuclear transport as an adjunctive therapy in the management of sepsis.
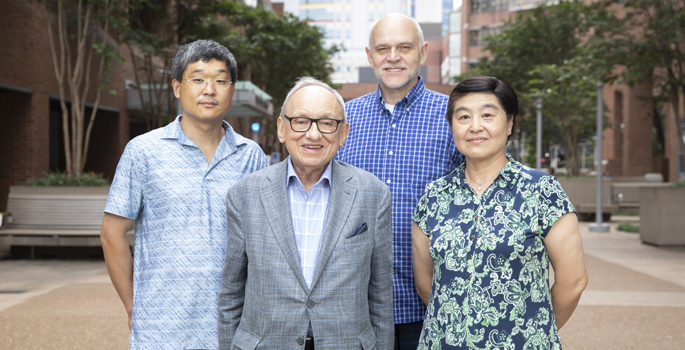
“Sepsis is fast and furious, especially among the youngest and oldest patients,” said senior author Jacek Hawiger, M.D., Ph.D., the Louise B. McGavock Professor, Distinguished Professor of Medicine and professor of Molecular Physiology and Biophysics at Vanderbilt.
“We hope that this new treatment will prove safe and effective not only in increasing survival but also reducing serious complications in survivors of sepsis,” said Hawiger, who also is a research health scientist at the Nashville Veterans Affairs Medical Center.
After his mother succumbed to sepsis, Hawiger was determined to find better ways to control and prevent it.
One way to restore physiologic barriers to sepsis and other inflammatory diseases is to deliver anti-inflammatory peptides and proteins across the cell membrane. During the past 20 years, Hawiger and his colleagues have pioneered platforms for doing so.
In the current study, they tested a peptide called a Nuclear Transport Modifier or NTM in an animal model of sepsis caused by spillage of the gut’s microbes into the bloodstream.
NTM not only suppressed production of pro-inflammatory factors but markedly reduced the amount of bacteria in the lungs and bloodstream even before antibiotic therapy was started. Signs of microvascular injury to the lining of tiny blood vessels were attenuated. And when NTM was combined with antibiotic therapy, survival nearly doubled.
“The study of nuclear transport signaling … opens up a new avenue for exploring innovative approaches to restore the complex balance of pro- and anti-inflammatory mechanisms in blood and vascular systems that would allow for successful recovery from sepsis,” the researchers concluded.
Ruth Ann Veach, research instructor in the Division of Nephrology, is first author. Co-authors include Yan Liu, M.D., Jozef Zienkiewicz, Ph.D., Lukasz Wylezinski, Ph.D., Kelli Boyd, Ph.D., DVM, and James Wynn, M.D.
The study was supported in part by National Institutes of Health grants DK058404, CA068485 and TR002243 and by a Veterans Affairs Merit Review Award.