Vanderbilt University researchers are closer to understanding the link between obesity, chronic inflammation and type 2 diabetes. Their findings may hasten development of new treatments for obesity-related diabetes, which is at epidemic proportions in the United States.
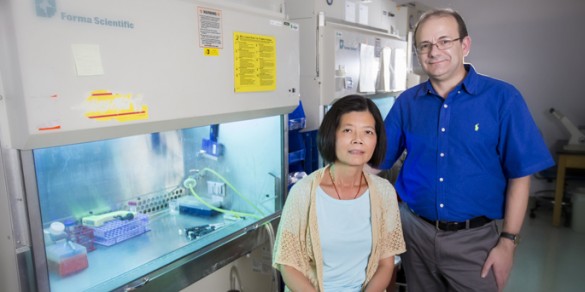
“There is still a long way to go,” cautioned Lan Wu, M.D., first author of a paper published this week by the Proceedings of the National Academy of Sciences. “You cannot design effective therapies without knowing what comes in, what goes out and ‘what’s cooking’ in the middle.”
This much is known: Accumulation of lipids in obesity triggers a low-grade inflammation that originates primarily from fat tissue. White blood cells (including lymphocytes), which normally fight infection and repair injury, are recruited to fat tissue and release small, powerful proteins called cytokines.
Some cytokines make matters worse. They fan the flames of inflammation and antagonize the action of insulin, the pancreatic hormone that stimulates uptake of circulating glucose by muscle, liver and other tissues. The result is tissue “resistance” to insulin, rising glucose levels, and type 2 diabetes.
In the current study, the Vanderbilt researchers found for the first time in the fat tissue of obese mice a subpopulation of innate-like regulatory B lymphocytes that secrete an anti-inflammatory cytokine called interleukin-10 (IL-10).
Recruited from the spleen, these cells are in short supply, however, and their anti-inflammatory capacity is impaired.
The researchers overcame this problem by isolating regulatory B lymphocytes from lean mice and transferring them into obese ones. The cells made their way to the fat tissue and released IL-10, which turned down the “slow burn” of inflammation and improved insulin sensitivity.
This suggests a regulatory B cell-based “therapy” could interrupt obesity-related inflammation and insulin resistance. But here’s where it gets complicated.
Two years ago, Wu, co-author Luc Van Kaer, Ph.D., and their colleagues reported the discovery of another set of innate-like lymphocytes in obese mice, called invariant natural killer T cells. They overproduce inflammatory cytokines that worsen insulin resistance.
These opposing effects represent the delicate balance of the body’s response to inflammation. In obesity, that balance becomes “tilted” in favor of inflammatory cytokines, explained Wu, research associate professor of Pathology, Microbiology and Immunology.
The goal of the research is to find a way to bring the inflammatory response back into balance. “You may not become lean,” she said, “but as long as you’re not sick, that’s still something.”
Certainly the best way to stop and even reverse type 2 diabetes in obese individuals is to lose weight. But strict diet and a vigorous exercise regimen are difficult for many people. “That’s why immunotherapy becomes an attractive alternative,” she said.
Van Kaer is the Elizabeth and John Shapiro Professor in the Department of Pathology, Microbiology and Immunology. Other co-authors were Vrajesh Parekh, Ph.D., Joseph Hsiao (now a fourth-year medical student at St. Louis University School of Medicine) and Daisuke Kitamura, M.D., of the Tokyo University of Science.
The research was supported in part by National Institutes of Health grants DK081536, AI070305 and HL089667.