Researchers in Vanderbilt’s Division of Nephrology conducted a Phase 3 clinical trial to test the safety and efficacy of a new drug to treat patients with end-stage renal disease.
Clinical trial results were published online in the Journal of the American Society of Nephrology(JASN) and indicate that the medication, ferric citrate, is safe and effective and is projected to actually reduce health care costs in this patient population.

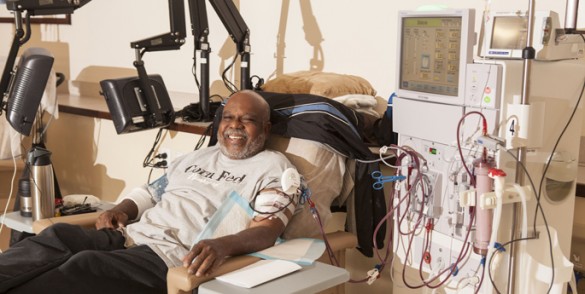
More than 400,000 patients in the United States are on dialysis to treat their kidney disease.
Dialysis patients usually have to take three different medications to overcome complications related to kidney disease: drugs that bind phosphorus in their food to reduce toxic buildup of the mineral in their bodies; erythropoietin-stimulating agents (ESA) that boost blood cell production; and intravenous (IV) iron.
Julia Lewis, M.D., Jamie Dwyer, M.D., Mohammed Sika, Ph.D., and colleagues in the Collaborative Study Group conducted a 441-patient randomized clinical trial to test the use of ferric citrate (Zerenex) to bind phosphorus, increase iron stores and reduce the usage of IV iron and ESA.
Patients were randomized to receive either ferric citrate or another phosphorus-binding agent for one year.
This was then followed by a four-week period in which patients taking ferric citrate were again randomized to either continue on the medication or switch to placebo.
The study investigators found that ferric citrate effectively reduced blood phosphorus levels while increasing iron stores and decreasing the need for IV iron and ESAs, thereby reducing the cost of treatment by $2,104 per patient per year in drug cost savings alone.
“Ferric citrate binds the phosphorus in food and also increases iron in the blood, and it allows patients to need less or no IV iron and medicines to make their bone marrow produce more blood cells,” said Lewis, professor of Medicine in the Division of Nephrology and Hypertension.
She also noted that patients on dialysis often experience many serious adverse medical events, many of which require hospitalization, and that ferric citrate was linked with fewer of these events compared with currently available phosphorus-binding medications.
“While benefiting patients, ferric citrate is estimated to also actually reduce the cost of caring for dialysis patients by reducing IV iron and ESA usage, as well as hospitalizations,” Lewis said.
Ferric citrate is expected to receive FDA approval in the fall and will be the only phosphate binder that effectively manages phosphate levels and also increases iron stores and decreases IV iron and ESA use.
Study co-authors include Dwyer, Sika, Mark Koury, M.D., Peale Chuang, M.D., Gerald Schulman, M.D., Mark Smith, M.D., Frederick Whittier, M.D., Douglas Linfert, M.D., Claude Galphin, M.D., Balaji Athreya, M.D., A. Kaldun Nossuli, M.D., Ingrid Chang, M.D., Samuel Blumenthal, M.D., John Manley, M.D., Steven Zeig, M.D., Katagal Kant, M.D., and Tom Greene, Ph.D.