
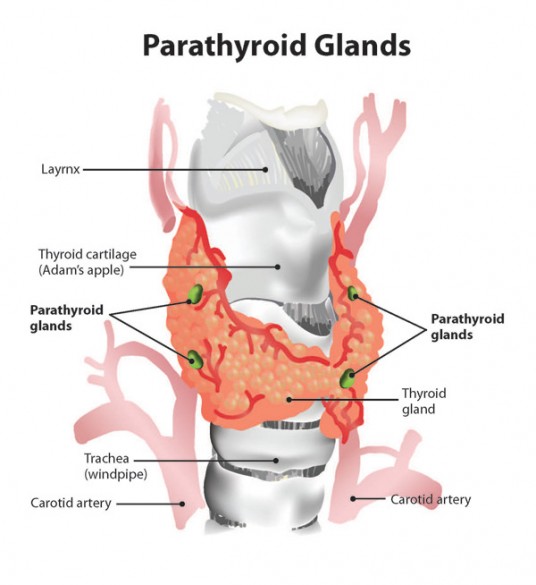
The parathyroid glands – four small organs the size of grains of rice located at the back of the throat – glow with a natural fluorescence in the near infrared region of the spectrum.
This unique fluorescent signature was discovered by a team of biomedical engineers and endocrine surgeons at Vanderbilt University, who have used it as the basis of a simple and reliable optical detector that can positively identify the parathyroid glands during endocrine surgery.
The report of the discovery of parathyroid fluorescence and the design of the optical detector was published in the June issue of the Journal of Biomedical Optics.
Damage to these tiny organs can have deleterious, life-long effects on patients’ health because they produce a hormone that controls critical calcium concentrations in bones, intestines and kidneys. However, the parathyroid glands are very difficult to identify with the naked eye. Not only are they small, but their location also varies widely from person to person and it takes a microscope to reliably tell the difference between parathyroid tissue and the thyroid and lymph tissue that surrounds it.
In 2004, more than 80,000 endocrine surgeries were performed in the United States and this number is projected to grow to more than 100,000 by 2020. Today, when a surgeon cuts into a patient’s neck to remove a diseased thyroid, somewhere between 8 to 19 percent of the time the patient’s parathyroid glands are also damaged or removed.
Parathyroid glow is surprisingly strong
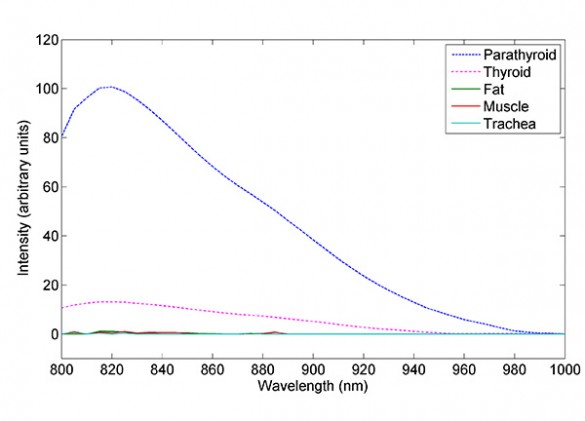
“We have discovered that the parathyroid glands are two to 10 times more fluorescent in the near infrared than any other tissues found in the neck,” said Professor of Biomedical Engineering Anita Mahadevan-Jansen, who directed the study. “We have taken measurements with more than 50 patients now and we have found this effect 100 percent of the time, even when the tissue is diseased. That is amazing. You almost never get 100 percent results in biological studies.”
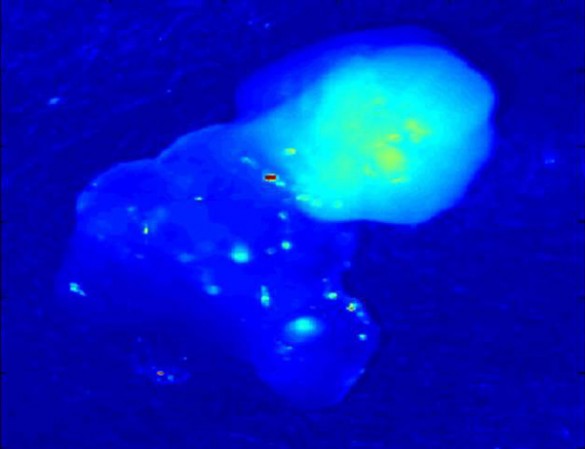
The fluorescence is so strong that it doesn’t take expensive or sophisticated instruments to detect. The Vanderbilt researchers have assembled a detector from off-the-shelf hardware. It consists of a low-powered infrared laser connected to an optical fiber probe. As the fiber connected to the laser illuminates the tissue with invisible near infrared light, other fibers in the probe are connected to a detector that measures the strength of the fluorescence that the laser excites. The university has applied for an international patent that covers this application.

“I was certainly impressed with how accurate this method seems to be,” said John Phay, an endocrine surgeon at the Ohio State University Medical Center, who collaborated in the study when he was at Vanderbilt. “The ability to detect the parathyroids would be a big help: The major problem in parathyroid surgery is finding them and it is very hard to avoid them in thyroid cancer surgery when you need to clear out lymph nodes.”
Using the first generation of the device was “a bit burdensome, because you have to dim the lights,” Phay commented. This will not be a problem with the next version, because it will include a filter that will block out visible light. According to the surgeon, the system will be the most useful with the planned addition of a camera that displays the fluorescence of all the tissues in the throat on a single display.
Project begins with curiosity of first-year surgery resident
The story of discovery began in 2007 when Lisa White, a first-year resident in the Vanderbilt surgery department, participated in her first neck surgery. “It was a very difficult case,” White said. “We were looking for the parathyroid glands and they were very hard to find, although we finally did find them. After the surgery was over, I decided that we really need a better way of identifying parathyroid tissue.”
This conclusion led White to conduct a literature search of the research that has been conducted on the basic physiology and biochemistry of the parathyroid. In the process she came across a paper written by Mahadevan-Jansen with another intern that described an optical technique that can detect liver cancer.
“I thought that if such a technique could detect the difference between normal and cancerous liver tissue, surely it could tell two different types of tissue apart,” White said. So she decided to pay Mahadevan-Jansen a visit.
“One afternoon there was a knock on my door. It was Lisa and she asked me about methods for detecting the parathyroid,” said Mahadevan-Jansen, whose research centers on the use of optical techniques for the detection of diseased tissue. “I was interested, particularly because the maternal side of my family has a history of thyroid problems. So I asked her if she would like to check it out.”
Initial attempts didn’t work
White agreed and they began working together even though they didn’t have any funding to support the project. They recruited Phay, who was an attending endocrine surgeon at the time and had access to animal tissue from other experiments being conducted on campus. They tried several different optical techniques, but none of the methods revealed anything distinctive about parathyroid tissue.
Finally, Mahadevan-Jansen decided to try a technique called Raman spectroscopy that fingerprints different organic molecules by subtle changes in the color of reflected light. The effect is very weak and difficult to measure.
When they put thyroid tissue in the instrument, they got a small signal. When they inserted parathyroid tissue, however, the detector saturated. This was totally unexpected because most biological fluorescence takes place in the ultraviolet and visible ranges. Biological molecules rarely fluoresce in the infrared region of the spectrum.
Possible light leak turned out to be a real effect
“At first, we thought it must be a light leak,” Mahadevan-Jansen said. When they kept getting the strong signal with several different samples, however, they realized that the effect was real.
Based on this success, Mahadevan-Jansen brought biomedical engineering graduate students Constantine Paras and Matthew Keller on board.

The expanded research team submitted an experimental protocol to Vanderbilt’s Institutional Review Board, which must approve all experiments involving animals or people. When it was approved, they gained access to human thyroid and parathyroid tissue.
“The parathyroid tissue from those first dozen patients kept saturating the Raman spectrometer so we had to keep reducing the laser’s intensity,” Mahadevan-Jansen recalled. “Finally, I realized that the instrument was saturating because the tissue was fluorescing.”
When she confirmed that this was happening, the engineer realized that they didn’t need the Raman spectroscope. All they needed was a light source in the near infrared and the right kind of near infrared detectors.
Cause of fluorescence remains a mystery
“We still haven’t figured out the source of the fluorescence, but that doesn’t stand in the way of using this effect to improve the effectiveness of parathyroid surgeries and reduce the damage done to the parathyroid in other endocrine surgeries,” Mahadevan-Jansen said.
Meanwhile, White is finishing up her final year as a resident in general surgery. She intends to make endocrine surgery a major part of her practice, so she could be one of the first surgeons whose patients will benefit from the discovery that resulted from her curiosity and initiative as a first-year intern.