
As many as 25 percent of hospital nurses go without sleep for up to 24 hours in order to adjust to working on the night shift, which is the least effective strategy for adapting their internal, circadian clocks to a night-time schedule.
That is one of the results of the first study to examine the strategies that night nurses use to adjust between day and night sleep cycles. The study was based on questionnaires from 388 nurses who work at the Vanderbilt University Medical Center and the results are published in the April 13 issue of the scientific journal, Public Library of Science One.
The study also found that variations in individuals’ circadian clock genes have a discernable impact on the nurses’ ability to adapt.
Disruptions to circadian rhythm unhealthy
A number of previous studies have found that repeated incidence of circadian misalignment – the condition that occurs when individuals’ sleep/wake patterns are out of sync with their biological clocks – is not healthy. Jet lag is the most familiar example of this condition. Circadian misalignment has been associated with increased risk of developing cardiovascular, metabolic and gastrointestinal disorders, some types of cancer and several mental disorders.
The way that nursing shifts have been scheduled since the nurse shortages of the 1980’s makes nurses particularly susceptible to this problem. Hospital nurses who work with inpatients do so almost exclusively in 12-hour shifts. The day shift normally runs from 7 a.m. to 7 p.m. and the night shift covers 7 p.m. to 7 a.m.
Vanderbilt night shift nurses typically work a schedule that includes three days on night shift followed by two to five days off, when most switch back to a normal sleep cycle. That means most of them are shifting sleep cycles as frequently as twice a week.

“I was very surprised to find that nurses’ second most frequent strategy was the ‘no sleep’ strategy that often involved staying awake for the 12 hours before starting the night shift,” said Karen Gamble, an assistant professor of psychiatry and behavioral neurobiology at the University of Alabama at Birmingham, who worked on the study as a post-doctoral fellow at Vanderbilt. “That means they are skipping sleep for at least 24 hours straight.”
Five distinct sleep strategies
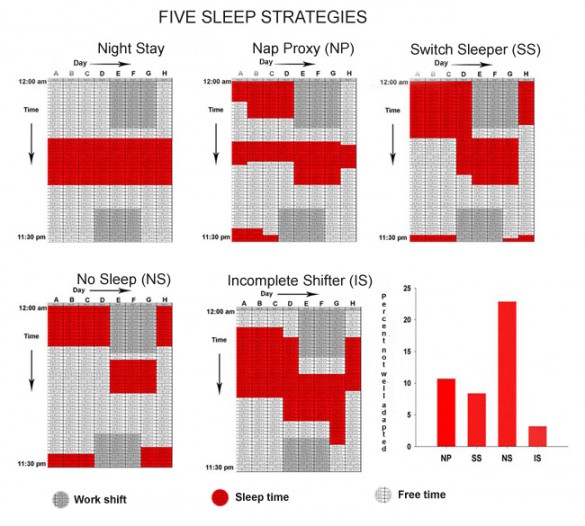
The researchers identified five distinct strategies that the nurses used to adjust their circadian clocks. The most common approach, used by about half the participants, was to sleep in late on the morning before their first night shift. A small percentage maintained a nighttime schedule on their days off. The other two strategies were intermediates.
“[rquote]It’s not often that you identify and characterize a human behavior for the first time, let alone one that has an effect on human health[/rquote],” said Vanderbilt graduate student and co-author Chris Ciarleglio.
It was beyond the scope of the study to determine the effect that the nurses’ sleep strategies have on their performance. “It’s very difficult to differentiate between the strategies and the individual variations of the people who choose them,” Gamble acknowledged.
However, the study did ask the nurses several questions designed to assess their adaptation. For example, they asked how well adapted they felt; how long it takes them to get out of bed; how much caffeine they use; and how likely they are to fall asleep during the day. The answers to these questions indicate that the nurses who use the sleep deprivation strategy are the most poorly adapted of the five groups.

The researchers recommend that nurses should be advised to avoid the “no sleep” strategy when working nights and suggest that hospitals re-evaluate the way that they schedule nurses to reduce the frequency with which nurses switch sleep schedules.
“Most people don’t want to work at night and those that do use what works best for them and their lifestyle,” observed co-investigator Nancy Wells, director of nursing research at Vanderbilt.
Scheduling is a very touchy issue and many nurses, particularly the younger ones, like the current system because it allows them to string together a number of days off without taking vacation, she added.
Genetics affect adaptation

The researchers also took DNA samples from all the participants to investigate the extent to which their circadian clocks influenced their adaptation. They determined the nurses’ “chronotype” – whether they are natural early risers (larks) or late risers (owls) – and which of seven well-known variations, or polymorphisms, in human circadian clock genes that each nurse possessed.
This information allowed the researchers to determine that larks adapt particularly well to day shifts and particularly poorly to night shifts, while owls do not adapt particularly well or poorly to either shift. In addition, they found that variants in one gene, called PER3, appear to have a major impact on the effectiveness of the no sleep strategy. Individuals with one variant of this genotype appear to respond more poorly than average to the strategy while those with the other genotype appear to respond better than average.
Vanderbilt Professor of Biological Sciences Carl Johnson, Alison Motsinger-Reif, assistant professor of statistics at Northern Carolina State University, Marshall Summar at Children’s National Medical Center in Washington, D.C. and Douglas McMahon, Vanderbilt professor of biological sciences, also contributed to the research.
The research was initially funded by Vanderbilt’s Discovery Grant program and then by a grant from the National Institute of Mental Health.
















